Lightning Talk + Poster ESA-SRB-ANZOS 2025 in conjunction with ENSA
Clinical audit of the polycystic ovary syndrome service at Monash Health (#198)
Objective: Polycystic ovary syndrome (PCOS) is the most common endocrinopathy in women of reproductive age (1). This complex disorder presents multisystemic health implications including reproductive, metabolic and mental health disorders. Monash Health established a comprehensive statewide PCOS service in November 2017. This study aims to examine the patients’ demographics, PCOS subgroup distribution, and prevalence of metabolic and mental health disorders among women attending the Monash Health PCOS service.
Methods: A retrospective audit was conducted of all patients (n=143) attending the Monash Health PCOS service between January 2024 to June 2024.
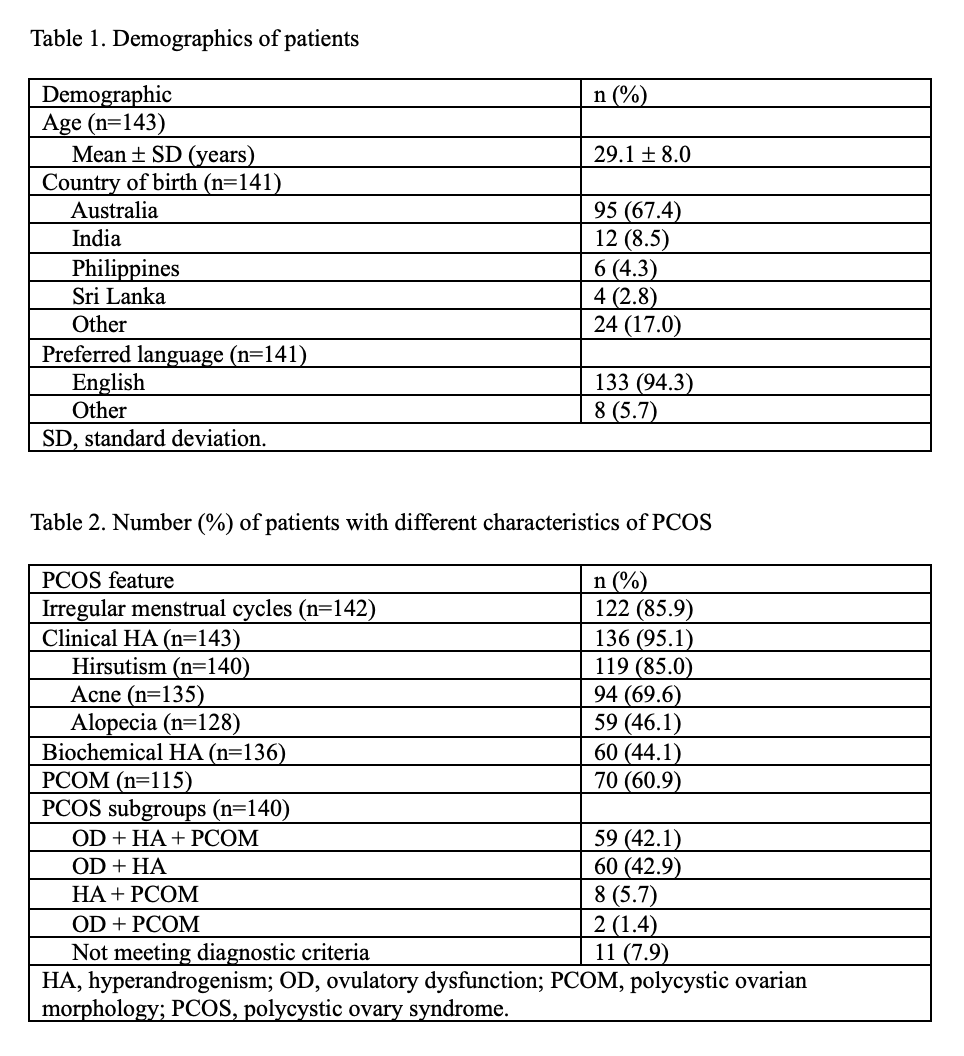
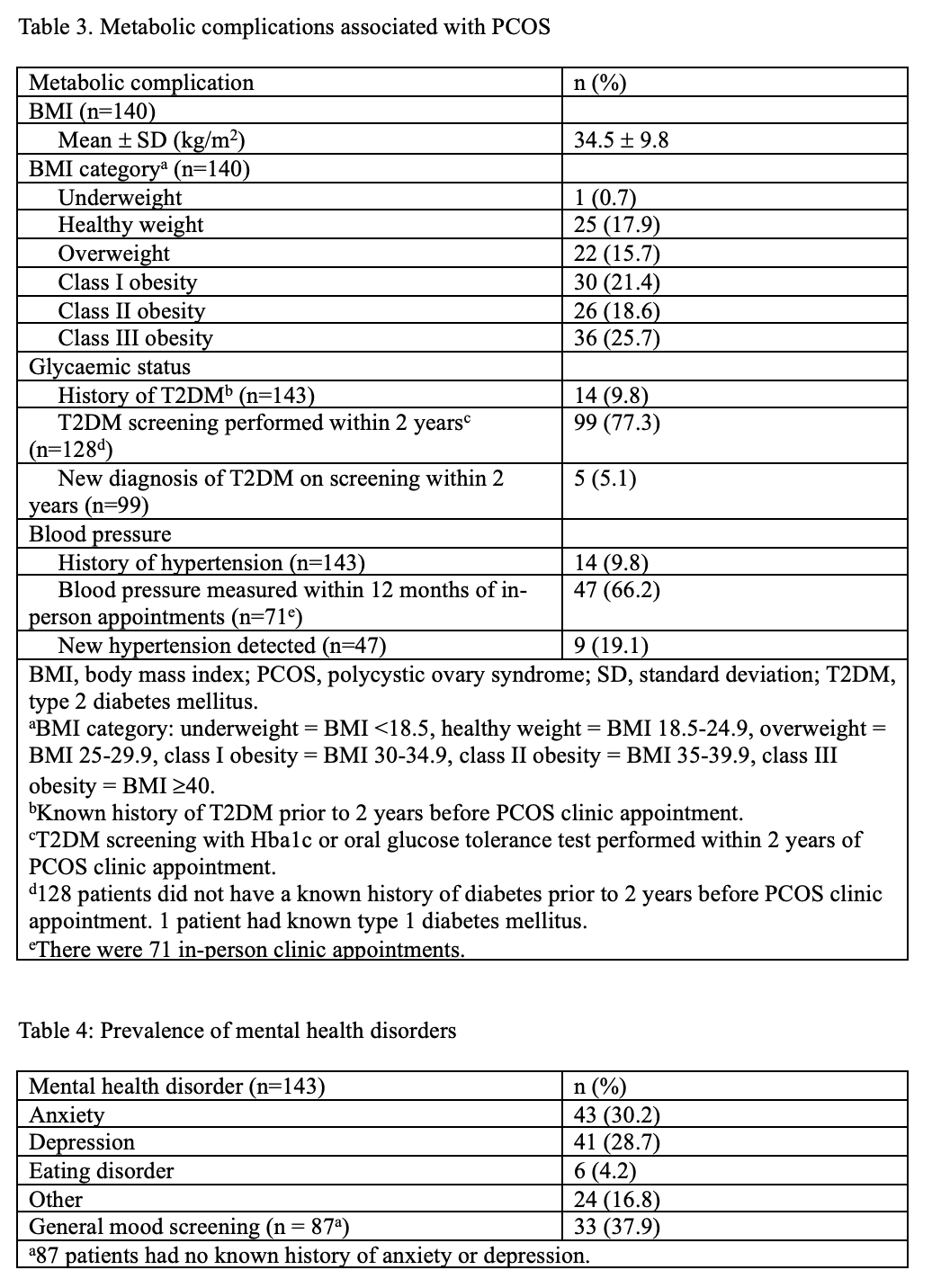
Results: 67.4% (n=95) of patients were born in Australia. Mean age was 29.1 (standard deviation [SD] 8.0) years. PCOS subgroup distribution revealed ovulatory dysfunction with hyperandrogenism as most prevalent at 42.9% (n=60). Obesity prevalence was 65.7% (n=92), with mean body mass index of 34.5 (SD 9.8) kg/m2. 9.8% (n=14) of patients have known history of type 2 diabetes mellitus (T2DM). Screening for T2DM within two years occurred in 77.3% (n=99) of patients without pre-existing T2DM, identifying new onset diabetes in 5.1% (n=5). 9.8% (n=14) of patients have known hypertension. Blood pressure measurement within the past year was documented in 66.2% (n=47) of in-person appointments (n=71), detecting new hypertension in 19.1% (n=9). The prevalence rates of mental health comorbidities were 30.2% (n=43) for anxiety, 28.7% (n=41) for depression and 4.2% (n=6) for eating disorders. General mood screening was documented in 37.9% (n=33) of patients without prior history of anxiety or depression (n=87).
Conclusion: This clinical audit confirms elevated metabolic and mental health comorbidity burden in women with PCOS attending specialised care. Despite established service provision, gaps remain in cardiovascular risk factor and mental health screening. Enhanced systematic screening protocols aligned with evidence-based guidelines are essential to optimise patient outcomes and reduce long-term complications in this high-risk population.
- Bozdag G, Mumusoglu S, Zengin D, Karabulut E, Yildiz BO. The prevalence and phenotypic features of polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod. 2016 Dec;31(12):2841–55.