Poster Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
Progressive Delays in Adrenal Venous Sampling for Regional Patients: A Single-Centre Experience in Far North Queensland (#120)
Adrenal Venous Sampling (AVS) is the definitive diagnostic modality for subtyping primary aldosteronism, enabling targeted surgical intervention in unilateral disease.¹ However, in regional centres such as Cairns Base Hospital, patients must be referred to tertiary facilities in Brisbane or the Gold Coast, introducing significant logistical and temporal barriers.
This study evaluated trends in AVS wait times and potential clinical implications of delayed access in a regional cohort.
A retrospective audit was conducted on patients referred for investigation of primary aldosteronism at Cairns Base Hospital between 2017 and 2024. Patients were identified via CaseMix coding and referrals for Seated Saline Suppression Testing (SSST). Exclusion criteria included normotensive results, alternative diagnoses, mortality, refusal, medical management, or incomplete investigations. Data were collected on demographics, biochemistry, comorbidities, antihypertensive burden, and AVS timelines.
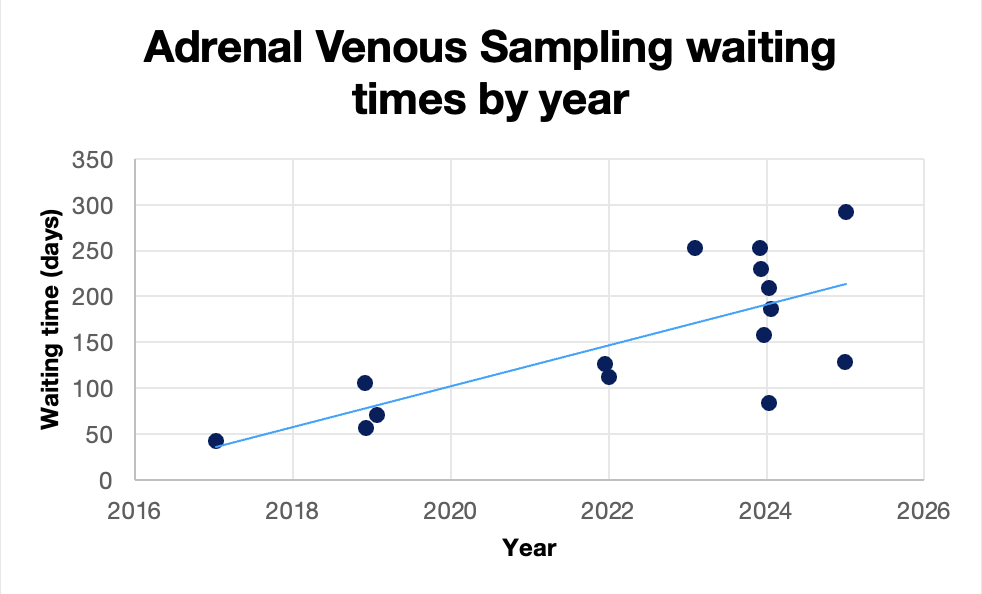
Of 63 identified patients, 16 underwent AVS and were included in the final analysis. The mean age was 55.4 years, and the mean aldosterone-to-renin ratio was 191.6. AVS wait times increased significantly over the audit period, from a mean of 68.75 days in 2017–2019 to 175.17 days from 2020 onward. Two patients developed hypokalaemia while awaiting AVS, requiring oral replacement. No macrovascular events were recorded. Common comorbidities included dyslipidaemia and smoking. Most patients (n=10) required three or more antihypertensive agents. While no association was observed between antihypertensive burden and AVS wait time, the majority had suboptimally controlled blood pressure—a well-established risk factor for cardiovascular disease, stroke, and metabolic complications including obstructive sleep apnea.²
AVS access delays are increasing for regional patients, with potential negative implications for clinical outcomes and healthcare resource utilisation. These findings support consideration of a locally delivered AVS service in Far North Queensland. In parallel, emerging evidence supporting non-invasive PET-based subtyping techniques warrants investigation in the Australian context to improve diagnostic equity and reduce reliance on tertiary AVS capacity.³
- 1. Faconti L, Kulkarni S, Delles C, et al. Diagnosis and management of primary hyperaldosteronism in patients with hypertension: a practical approach endorsed by the British and Irish Hypertension Society. J Hum Hypertens. 2024;38(1):8-18. doi:10.1038/s41371-023-00875-1 2. Mullen N, Curneen J, Donlon PT, et al. Treating primary aldosteronism-induced hypertension: novel approaches and future outlooks. Endocr Rev. 2024;45(1):125-170. doi:10.1210/endrev/bnad026 3. Zheng Y, Long T, Peng N, et al. The value of targeting CXCR4 with 68Ga-Pentixafor PET/CT for subtyping primary aldosteronism. J Clin Endocrinol Metab. 2024;109(1):171-182. doi:10.1210/clinem/dgad421