Oral Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
Beyond the Scale: Perspectives on Comprehensive Obesity Management in a Tertiary Multidisciplinary Service (128258)
 This study explores the lived experiences of individuals participating in the Tertiary Obesity Multidisciplinary Service, with a focus on the perceived value and impact of the support received beyond weight loss outcomes.
This study explores the lived experiences of individuals participating in the Tertiary Obesity Multidisciplinary Service, with a focus on the perceived value and impact of the support received beyond weight loss outcomes.
A qualitative approach was employed to examine patient experiences within the Tertiary Obesity Multidisciplinary Service (TOMS), which delivers integrated care through a group-based intervention for individuals with complex obesity. Thirteen participants took part in semi-structured interviews, which were transcribed and analysed in NVivo using Braun and Clarke’s (2006) theoretical thematic analysis framework.
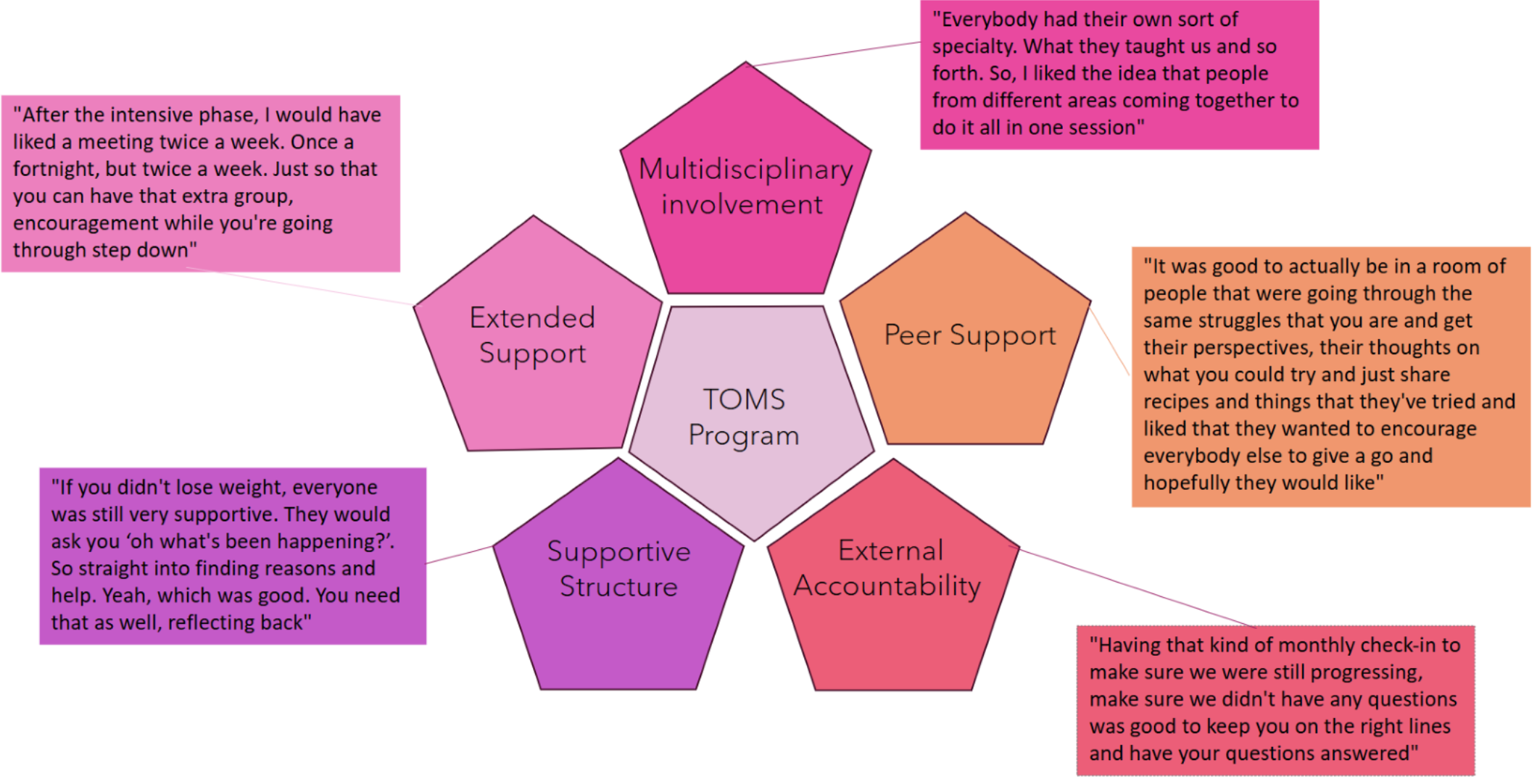
While participants initially engaged with TOMS for chronic disease management and surgical preparation, they reported that the most valued aspects of the program were the supportive structures, multidisciplinary team involvement, peer support, and external accountability. The program’s individualised and tailored care facilitated meaningful behaviour change, improved food literacy, and led to the development of sustainable healthy habits. Participants reported challenges in the stepdown phase due to reduced frequency of contact, which led to feelings of isolation and a loss of momentum. Participants suggested extended support and longer follow-up would be beneficial for long-term behaviour change and highlighted the importance of emotional and social support and motivation. Overall, participants described feeling happier, more energetic, and socially connected.
Findings suggest that multidisciplinary group programs like TOMS offer significant benefits beyond weight loss, particularly in promoting behavioural change and providing psychosocial support. These insights underscore the importance of incorporating patient perspectives into program design and highlight the value of integrated, person-centered care in managing complex obesity.