Poster Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
From Weight Loss to Waitlist: Evaluating the Impact of the Tertiary Obesity Multidisciplinary Service (#411)
To evaluate the effectiveness of the Tertiary Obesity Multidisciplinary Service (TOMS), a 12-month comprehensive weight-loss program designed to support individuals with complex obesity who face barriers to surgical access due to BMI or weight-related restrictions. Specifically, aiming to achieve weight or BMI goals for non-emergent surgical procedures through coordinated, multidisciplinary care.
Participants who commenced the TOMS program between January 2021 and April 2023 were followed until April 2025. Over the 12-month period, participants were supported by physiotherapists, pharmacists, psychologists, endocrinologists and dietitians to complete a Very Low Energy Diet (VLED), alongside structured education and exercise programs. Surgical waitlisting and operations were tracked for patients referred for pre-surgical weight loss. Key outcomes included surgery completion, avoidance, deferral with removal from the waitlist, and waitlisted status.
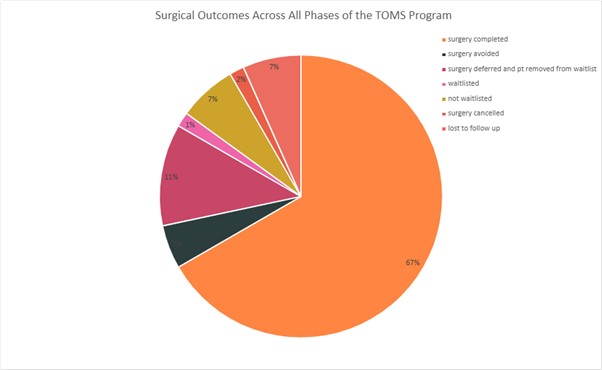
A total of 119 patients enrolled in TOMS during the study period. The mean age was 48.8 years (SD 13.7), and the median BMI was 46.4 kg/m² (IQR 40.5–54.8). Of these, 60 patients were referred to TOMS to improve access to non-emergent surgeries, including bariatric, oncological, hernia repair and orthopaedic procedures. Among them, 40 (67%) successfully completed surgery, 3 (5%) avoided surgery, 7 (12%) had surgery deferred and were removed from the waitlist, 1 (2%) had surgery cancelled, 1 (2%) remains waitlisted, 4 (6%) were not waitlisted, and 4 (6%) were lost to follow-up.
The TOMS program demonstrates that coordinated, multidisciplinary care can significantly improve access to non-emergent surgical procedures for individuals with complex obesity through meaningful weight loss. These findings underscore the value of a structured, multidisciplinary based approach in overcoming systemic barriers to surgery, enhancing patient readiness and supporting long-term health outcomes.