Oral Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
Losing Weight, Gaining Control: Diabetes Management Through TOMS (128313)
To evaluate the effectiveness of the Tertiary Obesity Multidisciplinary Service (TOMS)—a 12-month comprehensive weight-loss program involving physiotherapy, pharmacy, psychology, endocrinology, and dietetics—in improving glycemic control and reducing medication burden among individuals living with diabetes.
Participants with diabetes who commenced the TOMS program between January 2021 and June 2024 were included. Glycated haemoglobin (HbA1c) levels were collected at baseline, three, six and 12 months. Medication use, including insulin and sulfonylureas, was tracked throughout the program from documentation in the electronic medical record, with particular focus on adjustments during the intensive phase of the Very Low Energy Diet (VLED). Weight was tracked as a secondary outcome, collected at the same time.
Of the 73 participants included, 47% (n=34) were on insulin or sulfonylureas at baseline, with 11% on both. During the intensive phase, 89 insulin adjustments were recorded: 70% of participants reduced their insulin dosage, and 17% ceased insulin entirely. Additionally, 64% of participants discontinued sulfonylureas.
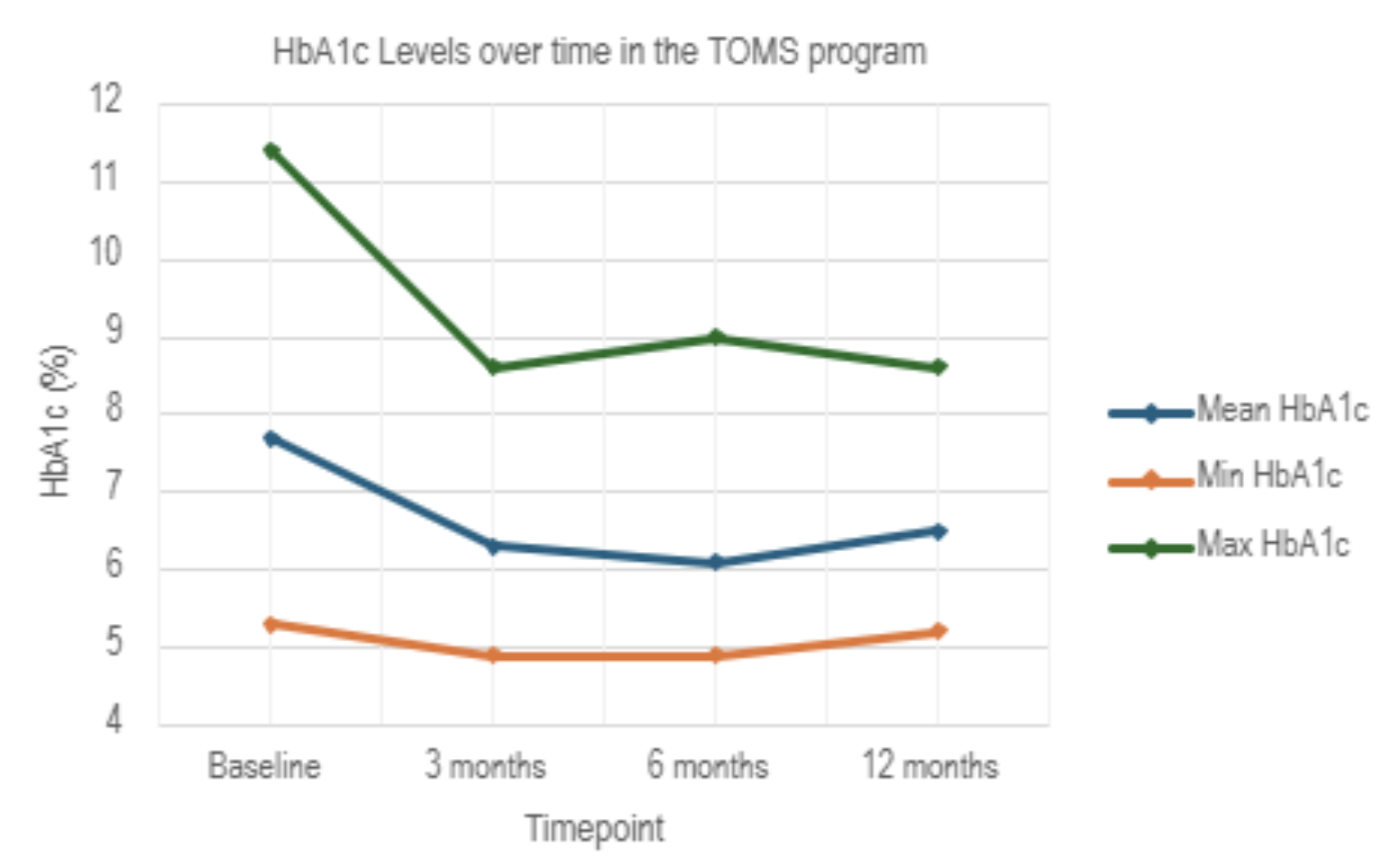
HbA1c levels showed significant improvement over time. Mean HbA1c decreased from 7.7% at baseline (n=71) to 6.4% at 3 months (n=63), 6.4% at 6 months (n=49), and 6.5% at 12 months (n=27). All reductions were statistically significant (p < 0.05), indicating sustained glycemic improvements.
All participants had a baseline BMI >35kg/m2 (mean = 147kg), with mean decrease in weight of 12.2% from baseline to 12 months.
The TOMS program demonstrates that integrated, multidisciplinary obesity care can lead to meaningful improvements in glycemic control, weight and a substantial reduction in diabetes medication burden. These findings highlight the value of coordinated care in managing complex obesity and enhancing metabolic health.