Oral Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
Does long-term calcium supplementation increase the risk of dementia? A post-hoc analysis from a 5-year randomised clinical trial of calcium supplements to prevent fractures in older women (128381)
Abstract
Calcium supplementation is commonly adopted to prevent and treat osteoporosis. Previous concerns around calcium supplements exacerbating vascular calcification and cardiovascular disease (CVD) have led to speculation around the potential negative impacts for dementia; given the strong nexus between vascular and cognitive health. However, data supporting such concerns are limited to observational studies (1, 2). This post-hoc analysis of a 5-year randomised controlled trial of calcium supplements evaluated its effect on the long-term risk for dementia in older women.
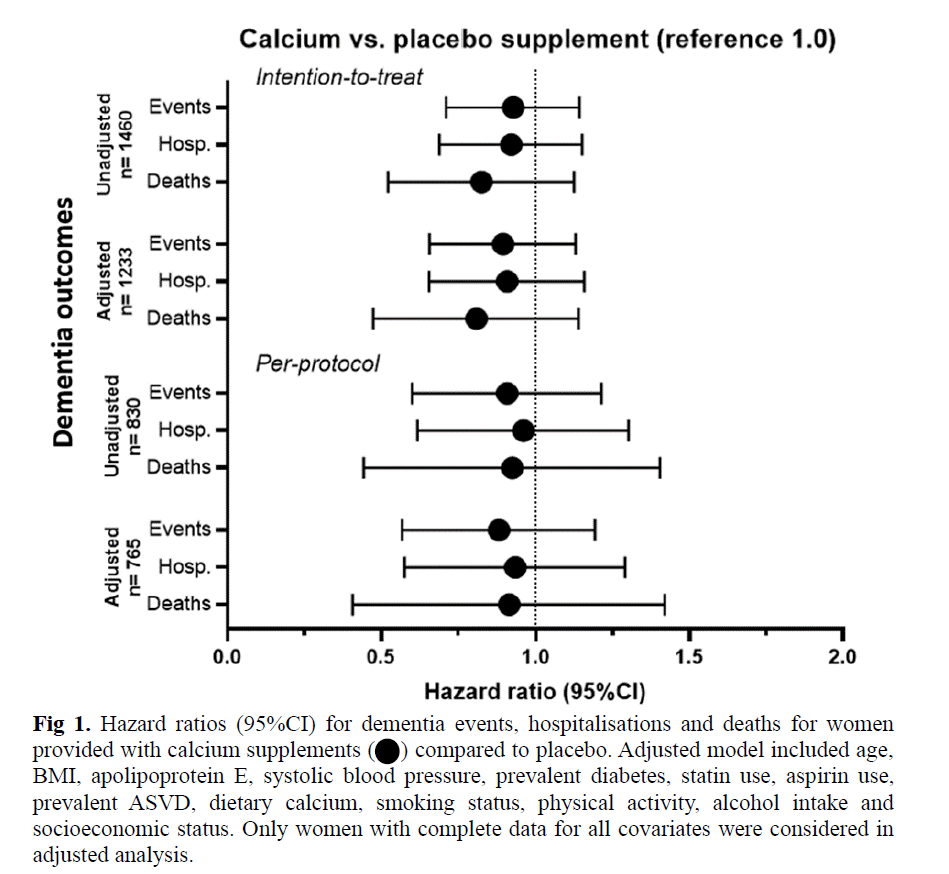
1460 dementia-free community-dwelling Australian women aged ≥70 years took part in the Calcium Intake Fracture Outcome Study (CAIFOS) in 1998. Women received either 1200 mg of calcium carbonate per day (n=730) or an identical placebo (n=730) for 5 years. The effects of calcium supplementation on dementia outcomes were examined using unadjusted and multivariable-adjusted Cox regression analysis under both intention-to-treat (ITT) and per-protocol criteria (PP, ≥80% annual tablet compliance, n=830). Dementia outcomes were obtained from linked hospital and mortality records from baseline over the next 14.5 years.
Mean age of women at baseline was 75.2 ± 2.7 years. Over 14.5 years, 269 women (18.4%) suffered a dementia event, comprising of dementia-related hospitalisations (n=243, 16.6%) and dementia-related deaths (n=114, 7.8%). Compared to placebo, calcium supplements were not associated with increased hazards for any of the dementia outcomes in unadjusted and multivariable-adjusted ITT and PP analysis (Fig 1). No significant differences in the cumulative dementia-free survival rates were observed between women randomised to calcium supplements or placebo for any dementia outcome (log-rank test, all p>0.05).
Five-years of calcium supplements did not increase the long-term risk for dementia in older women. Our findings support the safety of calcium monotherapy in relation to cognitive health in a population most likely to use and benefit from it due to their high risk for osteoporosis.