Poster Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
Lessons from a case series of diabetic ketoacidosis in dialysis patients (#161)
Diabetic ketoacidosis (DKA) is a life-threatening complication of diabetes mellitus, and while it is relatively uncommon in patients with end-stage renal disease (ESRD), its diagnosis and management in this population poses distinct challenges. (1) This case series aims to highlight the atypical presentation, and describe the altered pathophysiology, and complications from DKA treatment in individuals with diabetes undergoing dialysis.
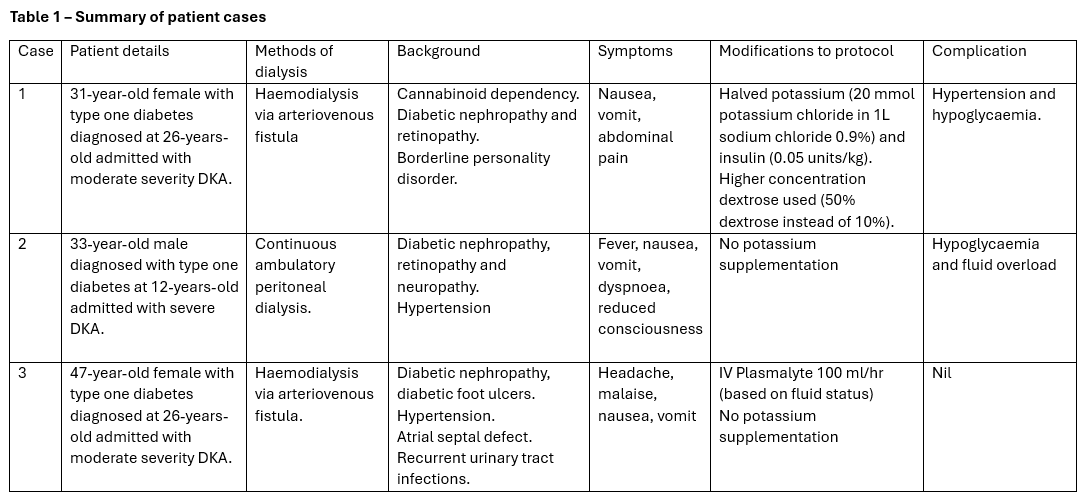
The cases are summarised in the table below. The hospital uses a fixed rate insulin infusion (0.1 units/kg/hr) DKA protocol, and all patients had some modification during their treatment (table 1). We noted that complications such as iatrogenic hypoglycaemia appeared higher in our case series participants compared to the general population treated with the same dose fixed rate insulin infusion protocol. (2)
The clinical features and biochemical presentation differ in our patient cohort due to altered pathophysiology. The key differences include (i) reduced and variable baseline urine output and absence of polyuria limiting the dehydration at presentation, (ii) potential correction of acidosis (but not insulin deficiency) at dialysis sessions and (iii) glucose-based dialysate contributing to hyperglycaemia in patients on peritoneal dialysis and (iv) significantly decreased insulin clearance, which protects against development of DKA in first place but also can lead to protracted hypoglycaemia during treatment. (3,4)
Despite the altered pathophysiology in development of DKA in dialysis patients, there is a lack of larger studies and most DKA guidelines do not address or provide specific guidance in this regard. With the small case series and brief review, we highlight the challenges in managing these patients and provide suggestions for an individualised approach including considerations of reduced intravenous fluid administration, judicious potassium replacement and lower insulin infusion rates which may help clinicians in managing such patients.