Oral Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
OPTIMAP: A Digitally Enabled Model to Transform Public Obesity Care in South Australia (128456)
Background
South Australia reports one of the highest obesity rates in Australia, with 13% of adults experiencing severe obesity (BMI >35). Until recently, the Royal Adelaide and Queen Elizabeth Hospitals operated siloed obesity services with a combined waitlist of over 700 patients and wait times exceeding seven years. In 2024, stakeholder engagement facilitated the unification of these services into a single multidisciplinary model—the CALHN Metabolic and Bariatric Clinic (CMBC), launched March 2025. The new model offers in-person and telehealth options, small group sessions (“My Healthier Life”), community-based exercise physiology, and fortnightly multidisciplinary team meetings.
Aim
To develop a sustainable, cost-effective digital model of care to improve access, service delivery, patient empowerment, and health outcomes.
Methods
Phase 1 – Discovery: An earlier prototype software (OBEMAN, CI-Wittert 2010) was assessed but not adaptable. Stakeholders (CMBC, CALHN Digital, Digivate Health) agreed to co-design a new solution: OPTIMAP.
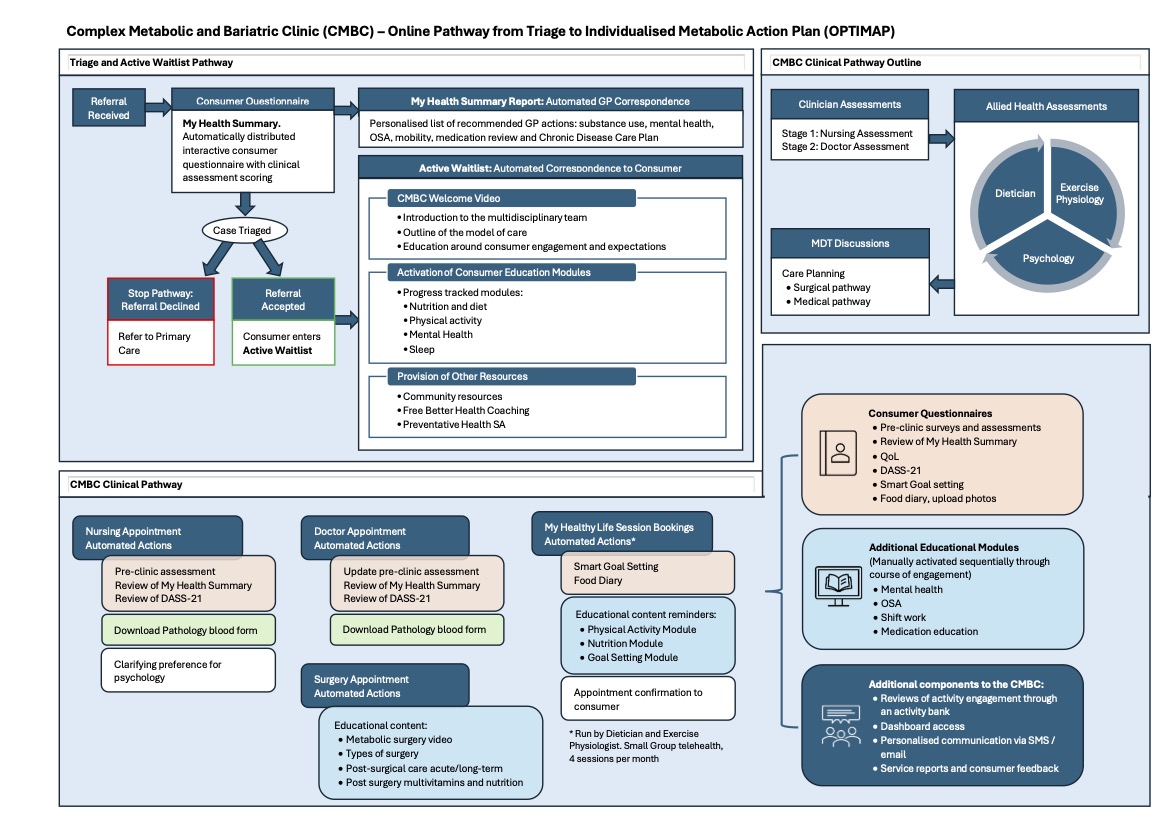
Phase 2 – Design: OPTIMAP (Online Pathway from Triage to Individualised Metabolic Action Plan) is a first-of-its-kind digital platform that:
- Triages patients by online questionnaire
- Provides pre-appointment education and coaching
- Generates GP-facing personalised "My Health Summaries"
- Delivers tailored content on diet, activity, sleep, mental health, medications, comorbidities and goal setting
- Automates documentation and pathology workflows
- Tracks real-time patient progress and surgical readiness
Phase 3 – Implementation: OPTIMAP launched in May 2025 following user testing.
Results
Within three months, the CMBC and OPTIMAP achieved a fivefold increase in physician and nursing activity and tripled dietetic capacity. First-appointment waitlist fell by 8.7%, maximum wait time reduced by two years, and failure-to-attend rates dropped by 65%. OPTIMAP improved referral compliance, clinical documentation and readiness tracking.
Conclusion
OPTIMAP and CMBC model represent a scalable, digitally enabled solution addressing systemic barriers in public obesity care. Ongoing KPI evaluation will inform future sustainability, equity and the broader health system impact.