Poster Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
Opioid-induced hypopituitarism in a young woman: case report (#163)
Opioids inhibit hypothalamic-pituitary function, commonly causing opioid-induced hypogonadotrophic hypogonadism and adrenal insufficiency(1,2). Chronic opioids suppress hypothalamic CRH and GnRH secretion via mu-opioid receptor inhibition(3,4).
We report a case of a 29-year-old woman with long-standing type 1 diabetes and autoimmune thyroiditis who has been on high dose opioids (up to 400-600mg/day tapentadol and 60mg/day oxycodone) for over four years for chronic abdominal pain.
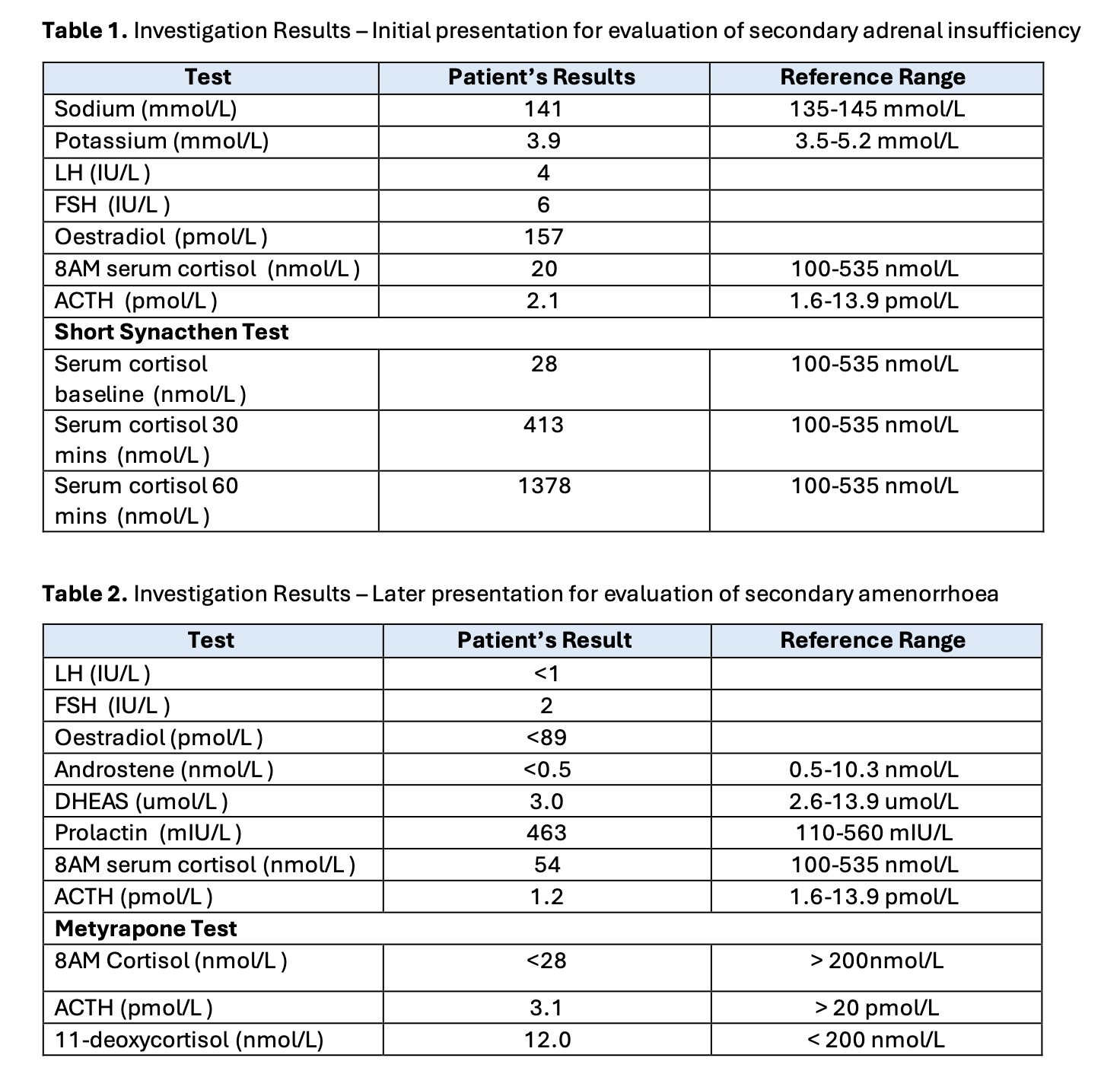
Patient presented with hypotension unresponsive to fluid resuscitation in 2024. Initial investigations revealed adrenal insufficiency with low morning cortisol (20 nmol/L) and low-normal ACTH (2.1 pmol/L). Serum sodium (141 mmol/L) and potassium (3.9 mmol/L) were within normal limits. Short Synacthen test demonstrated robust adrenal response (cortisol: baseline 28 nmol/L, rising to 413 nmol/L at 30 minutes, 1378 nmol/L at 60 minutes). Pituitary MRI showed no evidence of a structural abnormality related to the pituitary, and imaging showed normal adrenals. Hydrocortisone 10mg twice-daily was commenced with resolution of hypotension.
One year later the patient represented with secondary amenorrhea. Her BMI was 27.5 kg/m², with no signs of undernutrition. Investigations showed hypogonadotropic hypogonadism (LH<1 IU/L, FSH 2 IU/L, oestradiol<89 pmol/L), alongside persistent cortisol deficiency (54 nmol/L) with a suppressed ACTH (1.2 pmol/L). Metyrapone testing confirmed inadequate ACTH response (3.1 pmol/L) with low 11-deoxycortisol (12 pmol/L ) with adequate adrenal cortisol suppression (<28 nmol/L). Pituitary functional screening was otherwise unremarkable. Repeat pituitary MRI was normal. No cause of pituitary axis suppression was identified other than chronic opioid use. The patient was commenced on a combined oral contraceptive pill and referred to an outpatient chronic pain clinic.
This case demonstrates opioid-induced concurrent hypothalamic-pituitary-adrenal and gonadotropin axis suppression. Given increasing chronic opioid use, clinicians should screen for multi-axis pituitary dysfunction in patients on high-dose opioids, particularly young women, to ensure that appropriate and timely management of possible multiple suppressed hypothalamic-pituitary axes occurs.
- de Vries F, Bruin M, Lobatto DJ, Dekkers OM, Schoones JW, van Furth WR, et al. Opioids and Their Endocrine Effects: A Systematic Review and Meta-analysis. J Clin Endocrinol Metab. 2020 Apr 1;105(4):1020–9.
- Coluzzi F, LeQuang JAK, Sciacchitano S, Scerpa MS, Rocco M, Pergolizzi J. A Closer Look at Opioid-Induced Adrenal Insufficiency: A Narrative Review. Int J Mol Sci. 2023 Feb 26;24(5):4575.
- Fountas A, Van Uum S, Karavitaki N. Opioid-induced endocrinopathies. Lancet Diabetes Endocrinol. 2020 Jan;8(1):68–80.
- Rhodin A, Stridsberg M, Gordh T. Opioid Endocrinopathy: A Clinical Problem in Patients With Chronic Pain and Long-term Oral Opioid Treatment. Clin J Pain. 2010 Jun;26(5):374–80.