Poster Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
Filling the Gap for an Australian Cardiovascular-Kidney-Metabolic Training Program (#449)
Aims
Australia faces a rising burden of obesity and cardiometabolic disease, with disproportionately poor outcomes in First Nations and rural populations [1,2]. Medical obesity management has typically Endocrinology's domain, however Cardiology and Nephrology are developing interest. Despite increasing recognition of cardiometabolic syndrome, no formal Cardio-Kidney-Metabolic (CKM) training program exists. We aim to establish a structured, interdisciplinary program to address critical gaps in knowledge, care, equity, and outcomes.
Methods
To develop this proposal, we drew from local sub-specialty experts and international CKM programs, examining curriculum structures and training models [3,4]. Key elements such as advanced diagnostics, therapeutic strategies, mentorship frameworks, and cultural competency were considered.
Results
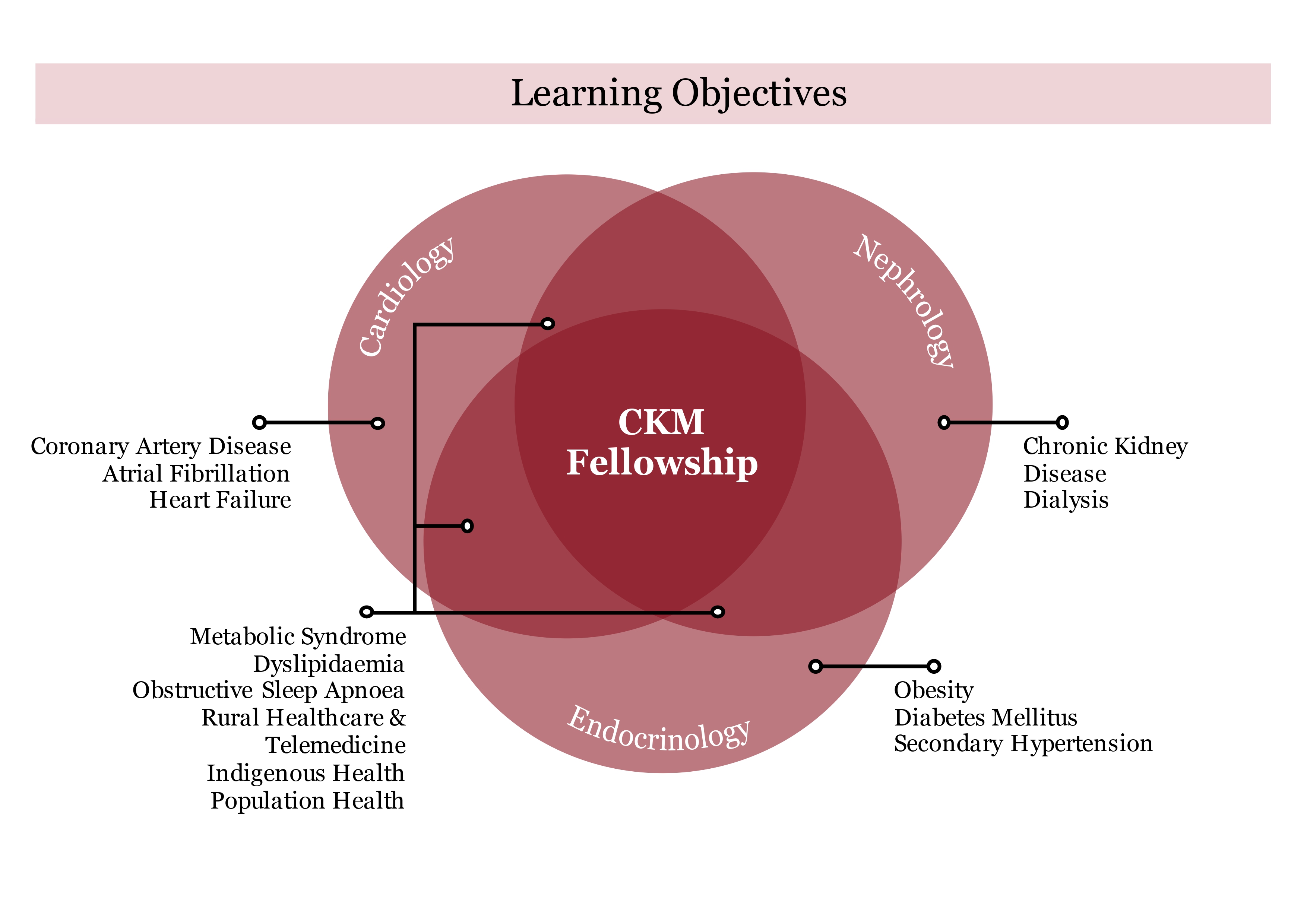
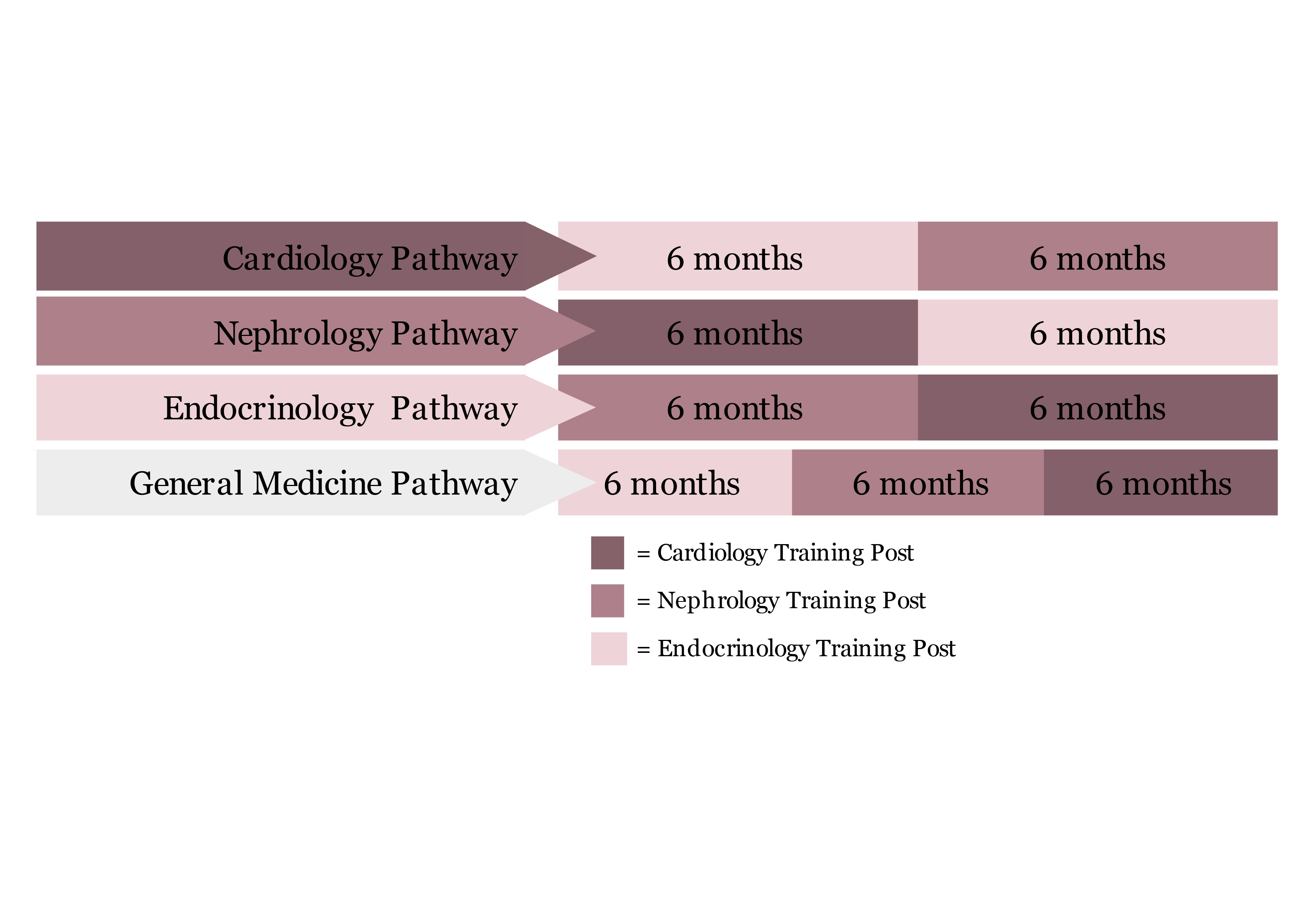
Insights from proposed global programs emphasise the importance of a comprehensive curriculum, integrating cardiology, nephrology, and endocrinology over 12 months. This would be offered to trainees from any of these specialties, as well as general physicians (requiring 18 months), with 6 months spent in each rotation outside their primary training program. Essential components include clinical rotations, community-based training, and research opportunities. Specialised obesity clinics during the endocrinology term will facilitate familiarity and expertise in managing type 2 diabetes, metabolic syndrome and its many complications, whilst chronic renal failure and cardiovascular risk management will be explored in-depth during their respective rotations. Cultural immersion experiences would foster relevant Indigenous health expertise, while digital health solutions would improve access in remote areas. A structured mentorship framework would support professional development. We will seek accreditation through the Royal Australasian College of Physicians to formalise this within Australian medicine.
Conclusion
An Australian CKM fellowship represents a transformative step toward bridging healthcare gaps, addressing disparities and equipping specialists with the skills to manage complex multi-system conditions. Establishing this program will improve interdisciplinary patient care and drive equitable health outcomes for patients living with obesity and cardiometabolic syndrome across Australia.
- 1. Paige E, Welsh J, Agostino J, Calabria B, Banks E, Korda RJ. Socioeconomic variation in absolute cardiovascular disease risk and treatment in the Australian population. Preventive Medicine. 2018 Sep 1;114:217-22.
- 2. Brown A, Carrington MJ, McGrady M, Lee G, Zeitz C, Krum H, et al. Cardiometabolic risk and disease in Indigenous Australians: the heart of the heart study. International journal of cardiology. 2014 Feb 15;171(3):377-83
- 3. McCarthy CP, Chang LS, Vaduganathan M. Training the next generation of cardiometabolic specialists. Journal of the American College of Cardiology. 2020 Mar 17;75(10):1233-7.
- 4. Saxon DR, Reiter-Brennan C, Blaha MJ, Eckel RH. Cardiometabolic medicine: development of a new subspecialty. The Journal of Clinical Endocrinology & Metabolism. 2020 Jul;105(7):2095-104.