Poster Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
Bone health in heart transplantation: a Melbourne perspective revealed a higher rate of post-transplant fractures in females which occurred earlier than in males despite antiresorptive therapy and preserving bone density those who received it. (#140)
To evaluate bone health outcomes of cardiac transplant recipients given the known bone density loss and fragility fractures in this cohort (1). The primary outcome was effect of antiresorptive therapy (treatment) on incidence of post-transplant fragility fractures. Secondary outcomes included the treatment impact on bone mineral density (BMD) and adverse events.
This retrospective cohort study included 196 adult patients (mean age 48 ± 12.9 years; 30.1% female) who underwent heart transplantation between 2012 and 2021 at the Alfred Hospital in Melbourne. Patient data were extracted from medical records.
Fragility fractures occurred in, 21 patients (10.7%) with a post-transplant fracture rate of 9.2% (18 patients).
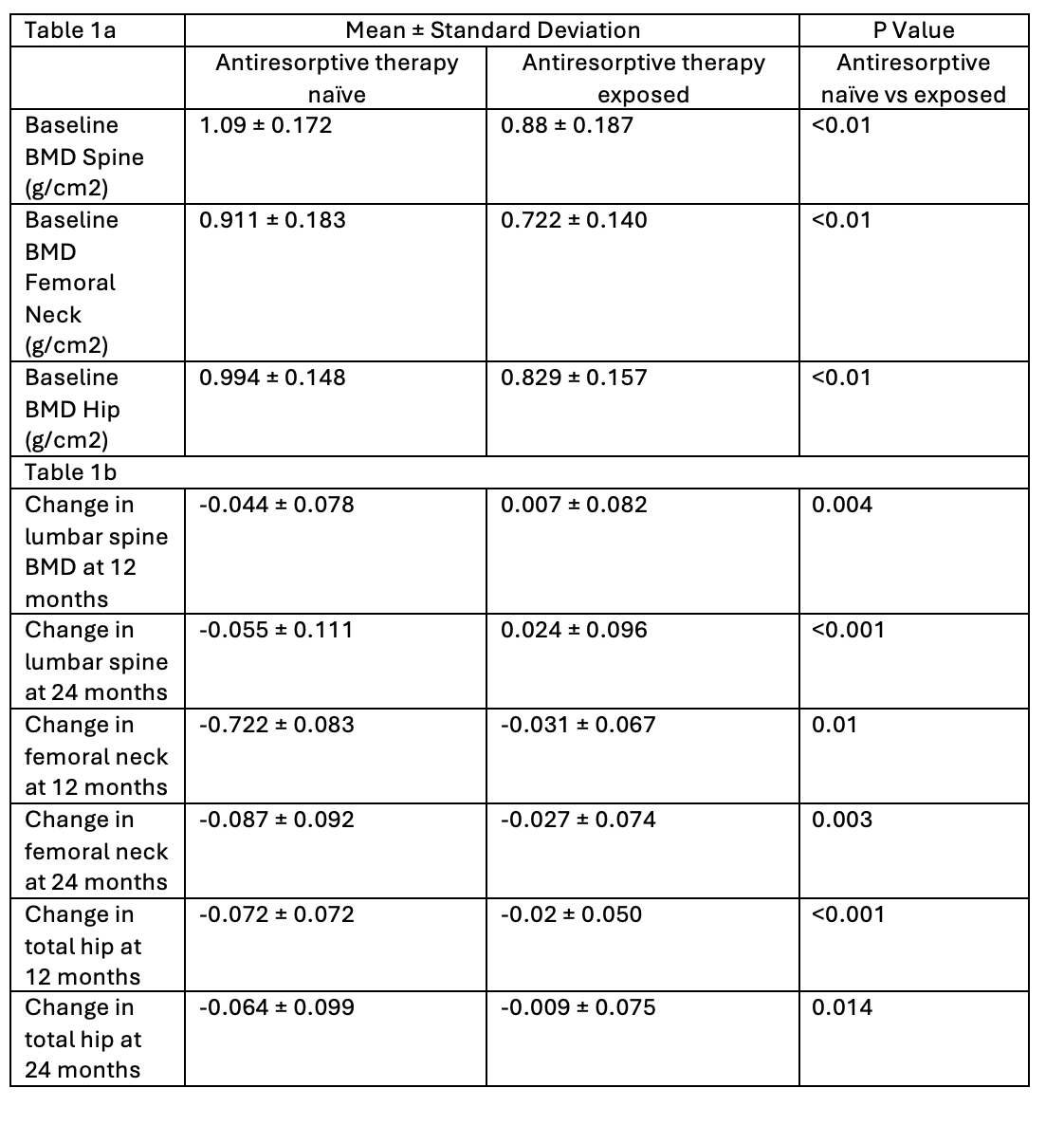
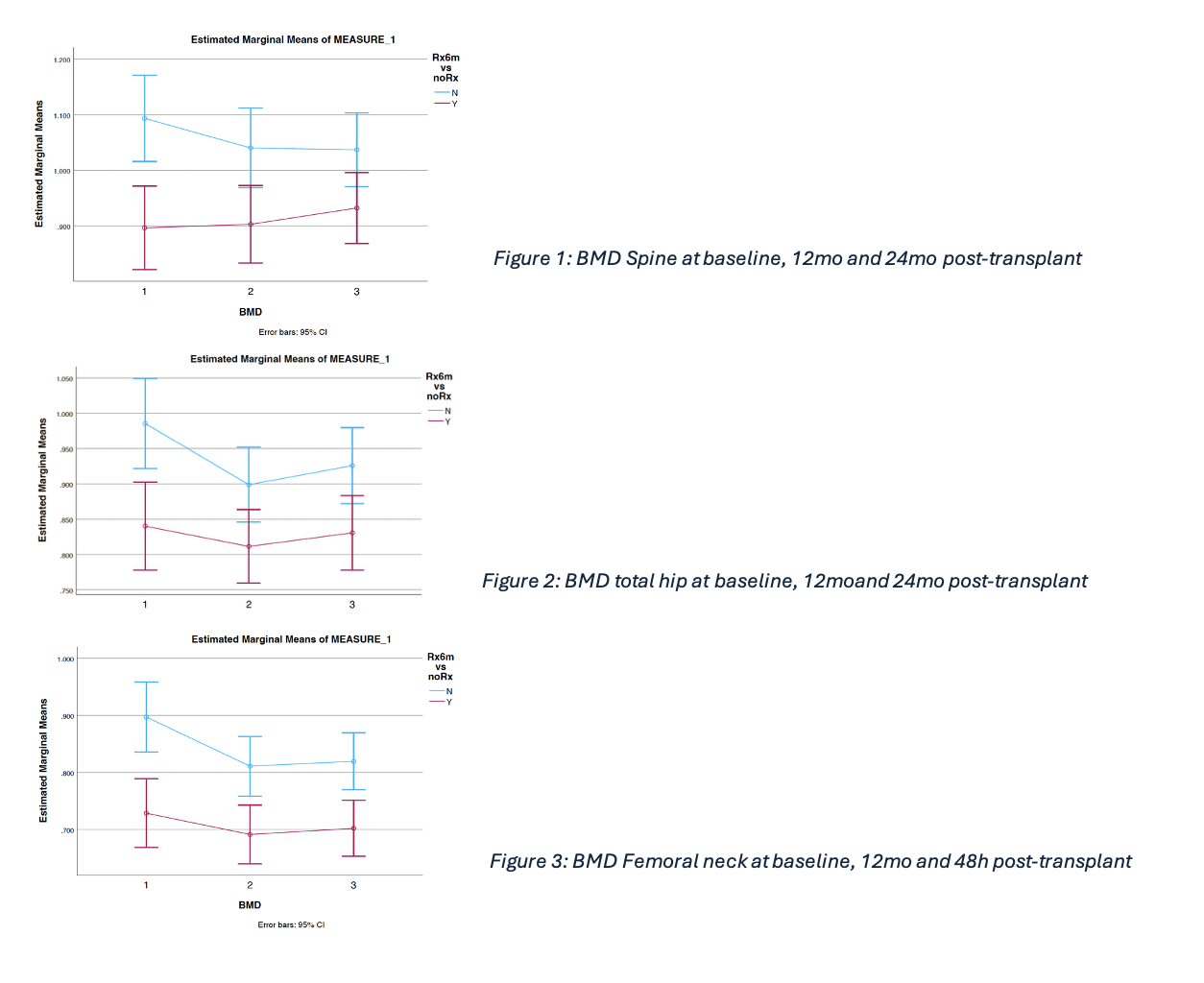
Those treated had significantly lower baseline BMD (Table 1a). Treatment attenuated BMD loss at 12- and 24-months post-transplant at all sites (Table 1b) but fracture rates were equal in both treatment-naïve (9.2%, 7/76) and treatment-exposed (9.4%, 11/117) groups. Treatment naïve patients lost BMD most significantly in the first 12 months after transplant, with 4% BMD loss in the spine (figure 1), 7% in total hip (figure 2) and 5% in femoral neck (figure 3) compared with those treated (95% CI 0.26 range, p<0.001).
Females fractured significantly more often and earlier than males (19.0% vs 5.2%, p = 0.006) (mean fracture-free survival 3,295 vs 3,918 days, p=0.001) even after adjusting for age, rejection rates and treatment.
In this real-world cohort, antiresorptive therapy attenuated BMD loss but did not reduce fracture incidence in adult heart transplant recipients, likely due to selection bias where high risk patients were preferentially treated. Female recipients had a higher and earlier risk of fractures.
These findings support a need for proactive bone health management in cardiac transplant recipients, particularly for female patients who represent a vulnerable and high-risk group. This is in line with international guidelines’ recommendations for an individualised approach (2).
- Leidig-Bruckner G, Hosch S, Dodidou P, Ritschel D, Conradt C, Klose C, et al. Frequency and predictors of osteoporotic fractures after cardiac or liver transplantation: a follow-up study. The Lancet. 2001;357(9253):342-7.
- Velleca A, et al. The International Society for Heart and Lung Transplantation (ISHLT) guidelines for the care of heart transplant recipients. J Heart Lung Transplant. 2023 May;42(5):e1-e141. doi: 10.1016/j.healun.2022.10.015. Epub 2022 Dec 20. PMID: 37080658.