Poster Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
I CAHn't believe that sodium (#171)
CB, a 45-year-old woman presented as an ambulatory patient to the Emergency department with intractable vomiting that escalated over two weeks, having coincided with escitalopram commencement. On examination she was haemodynamically stable and initial biochemistry revealed profound hyponatraemia (serum sodium 97 mmol/L), hyperkalaemia (serum potassium 6.1 mmol/L), bicarbonate 16 mmol/L, urea 4.1 mmol/L and creatinine 71 umol/L.
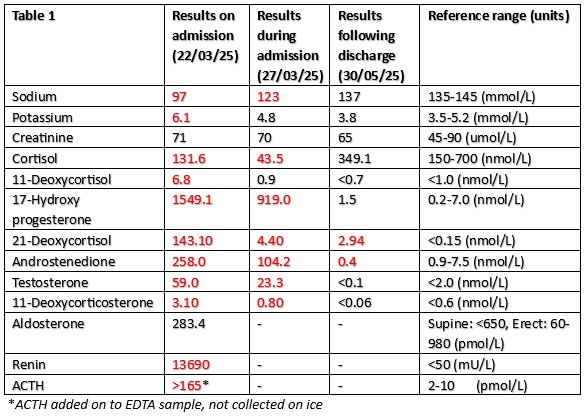
CB was diagnosed with simple virilizing congenital adrenal hyperplasia at birth with ambiguous genitalia and usually maintained on fludrocortisone 100 mcg and prednisolone 1mg daily. However, she had omitted these for three months, with intermittent compliance for 5 years. She reported longstanding secondary amenorrhea and hirsutism. Deranged androgen profile was documented during her admission (table 1).
CB was managed with intravenous hydrocortisone 100mg, 3% sodium chloride (NaCl) 3mg/kg, 0.9% NaCl infusion and reactive desmopressin use. She was admitted to the Intensive Care Unit for three days.
CB had hypovolaemic hyponatraemia which reflects a true sodium and water deficit. This was multi-factorial, including chronic aldosterone and cortisol deficiency; elevated ACTH; escitalopram commencement; and vomiting(1-3).
CB was at high risk of osmotic demyelination syndrome to very low initial serum sodium (≤105mmol/L) and several reversible cause of hyponatraemia(4). Guidelines recommend a serum sodium increase of 5mmol/L in the first hour, not exceeding 10mmol/L in 24 hours(1). There is no randomised controlled trial data regarding severe, chronic, hypovolaemic hyponatraemia so recommendations to replenish salt and water with isotonic saline are based on pathophysiology(1). Evidence on proactive vs reactive desmopressin use is conflicting(4-6).
CB’s post-discharge bloodwork reflects remarkable improvements of the androgen synthesis biomarkers and normalisation of serum sodium and potassium. She made a full recovery and reports strict adherence with medications.
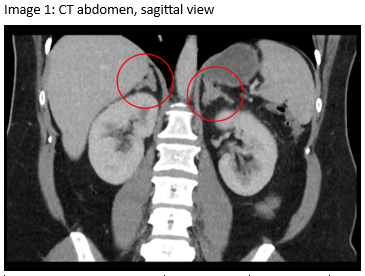
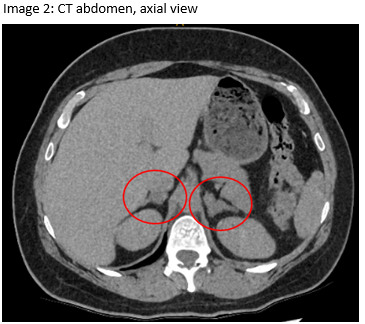
An outpatient CT abdomen revealed bilateral macronodular and heterogeneously low-density adrenal glands (Images 1, 2). Genetic studies are underway to confirm compound heterozygosity.
- Spasovski G, Vanholder R, Allolio B, Annane D, Ball S, Bichet D, et al. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Intensive Care Medicine. 2014;40(3):320-31.
- Noda M, Matsuda T. Central regulation of body fluid homeostasis. Proceedings of the Japan Academy Series B, Physical and biological sciences. 2022;98(7):283-324.
- Adrogué H, Tucker B, Madias N. Diagnosis and Management of Hyponatraemia: A Review. JAMA. 2022;328(3):280-91.
- Sood L, Sterns R, Hix J, Silver S, Chen L. Hypertonic saline and desmopressin: a simple strategy for safe correction of severe hyponatraemia. American Journal of Kidney Diseases. 2013;61(4):571-8.
- Achinger S, Ayus J. Use of Desmopressin in Hyponatraemia: Foe and Friend. Kidney Medicine. 2019;1(2):65-70.
- Spasovski G. Hyponatraemia-treatment standard 2024. Nephrology Dialysis Transplantation. 2024;39:1583-92.