Withdrawn Post Notification ESA-SRB-ANZOS 2025 in conjunction with ENSA
Adrenocortical carcinoma: a challenging cancer (#173)
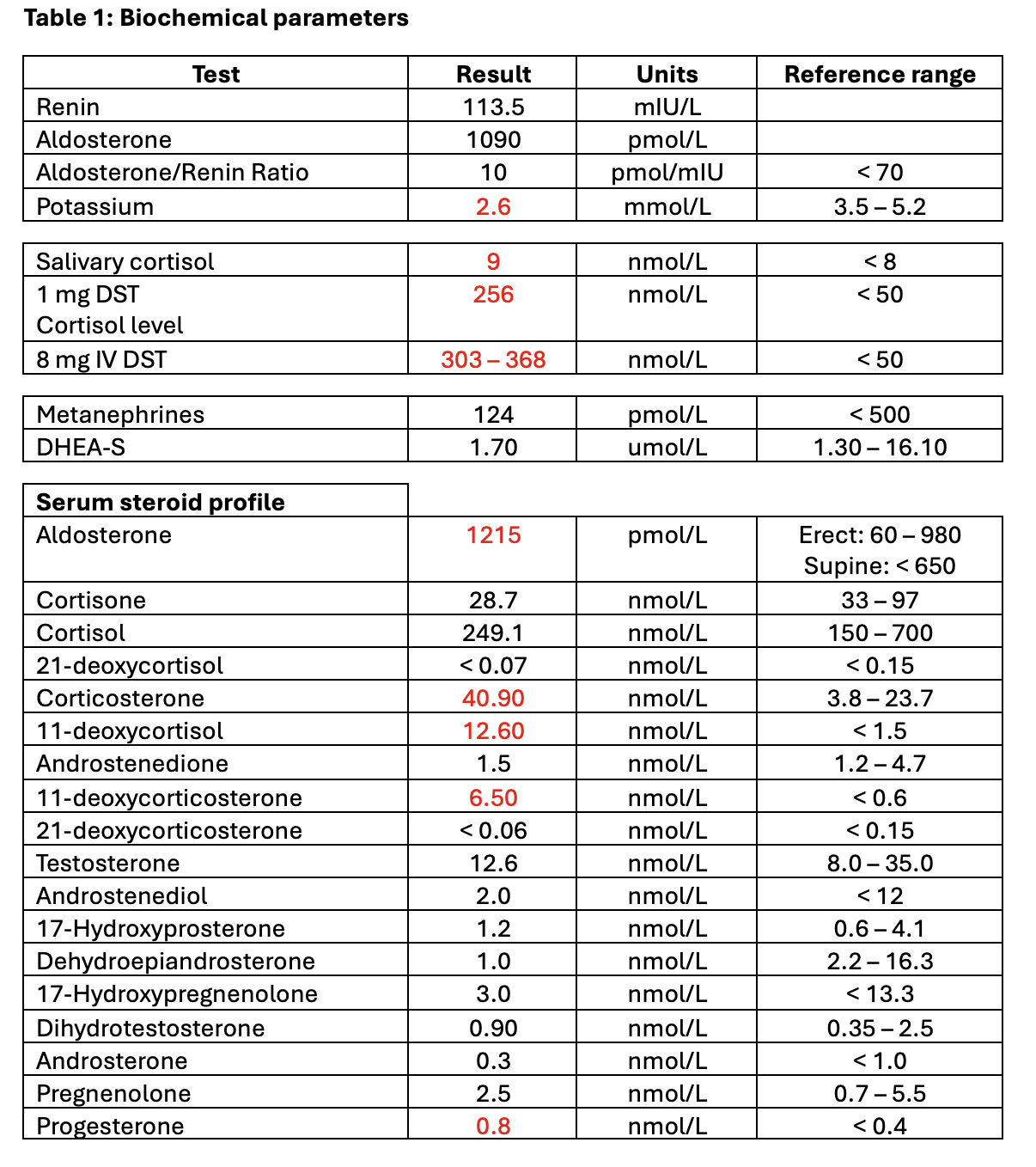
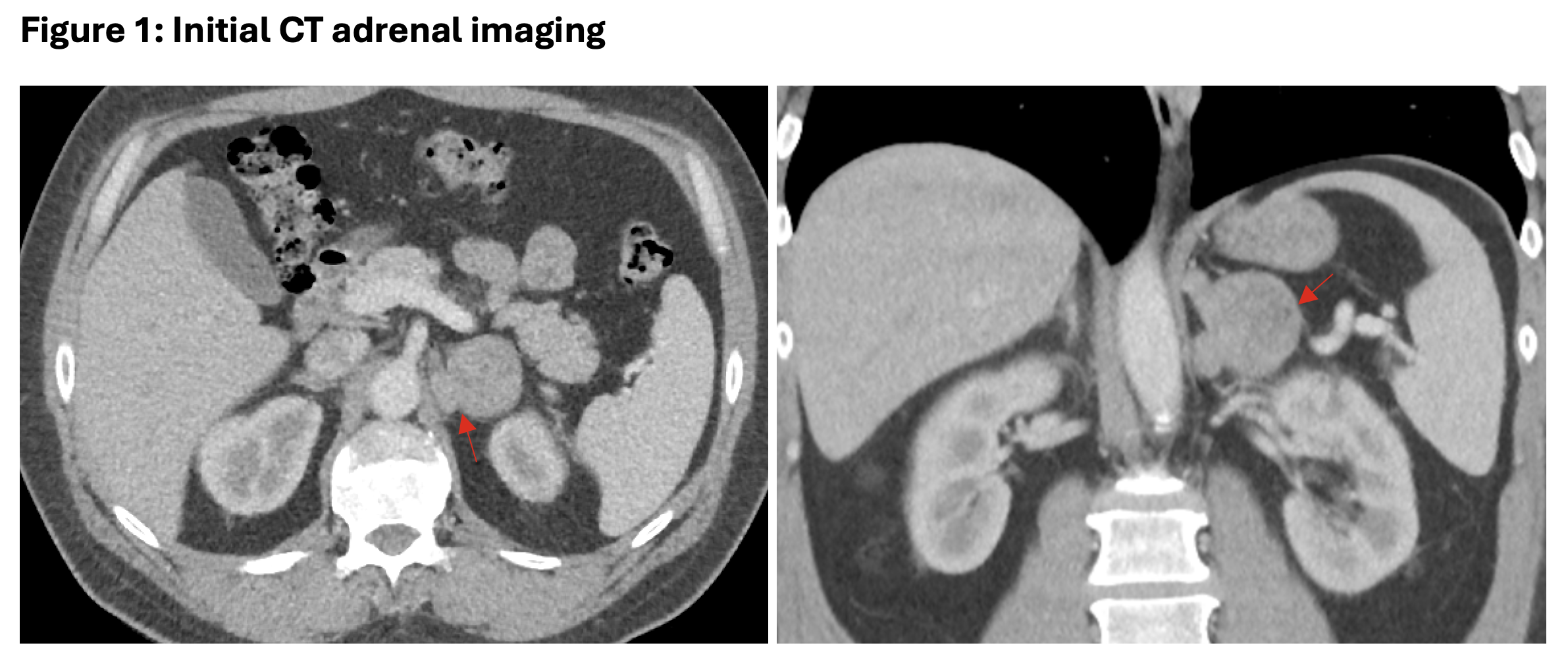
We present a previously well, 45-year-old man referred to Endocrinology from a regional centre for management of new-onset severe hypertension, hypokalaemia, and left adrenal mass. Baseline medications included verapamil, moxonidine, and potassium replacement. Initial external imaging (Figure 1) reported a 45mm lipid-rich left adrenal adenoma, however, subsequent reassessment of the imaging in our MDM noted concerning features (central heterogeneity, irregular morphology and satellite lobulation), prompting admission to our hospital. Full endocrine workup was completed (Table 1), noting profound hypokalaemia, non-suppressed dexamethasone suppression testing and elevated steroid precursors in the serum steroid panel. Repeat CT two months after initial imaging demonstrated interval growth of the adrenal mass – now measuring 62mm, abutting the diaphragmatic crus, inferior adrenal vein, and left kidney, favouring adrenocortical carcinoma (ACC).
The patient underwent urgent open left adrenalectomy. Histopathology confirmed high-grade ACC involving soft tissue and venous shave margins; ENSAT stage III (T3N0M0) with very-high risk disease (58mm tumour, R1 resection, Ki67>85% in hotspots and high mitotic rate. The patient commenced adjuvant mitotane, radiotherapy, and chemotherapy (carboplatin/etoposide).
Two months postoperatively, the patient developed worsening hypertension and hypokalaemia and was diagnosed with hepatic and pulmonary metastases. The patient completed radiotherapy and continues mitotane/carboplatin/etoposide.
ACC is a rare and aggressive disease – early diagnosis and referral to an experienced centre is crucial as delays can lead to poor outcomes. Diagnostic workup includes comprehensive hormonal evaluation and imaging to differentiate between adenoma from ACC. Liquid chromatography/mass spectrometry can characterise the steroid profile. ACCs typically secrete high levels of steroid precursors due to downregulation of several steroidogenic enzymes, whereas adrenocortical adenomas primarily produce cortisol (1). Complete resection is the only curative treatment. Adjuvant therapy is indicated in those with adverse prognostic features or advanced disease. Patients with metastatic disease have poor prognosis, with 5-year disease-free survival of 15% (2).
- 1. Yu K, Athimulam S, Saini J, et al. Serum steroid profiling in the diagnosis of adrenocortical carcinoma: a prospective cohort study. J Clin Endocrinol Metab 2024
- 2. Fassnacht, Martin et al. Adrenocortical carcinoma: a practical guide for clinicians (2025). The Lancet Diabetes & Endocrinology, Volume 13, Issue 5, 438 - 452