Poster Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
Corticotrophin-independent hypercortisolism in a patient with bilateral adrenal adenoma: Diagnostic and therapeutic conundrum (#176)
Hypercortisolism due to bilateral adrenal disease is an uncommon but challenging entity in endocrine practice. Despite the absence of overt clinical phenotypes, consequences of prolonged mild hypercortisolism can be profound. These include higher risk of diabetes, hypertension, osteoporosis and cardiovascular mortality; however, distinguishing these from general population risk is often difficult.
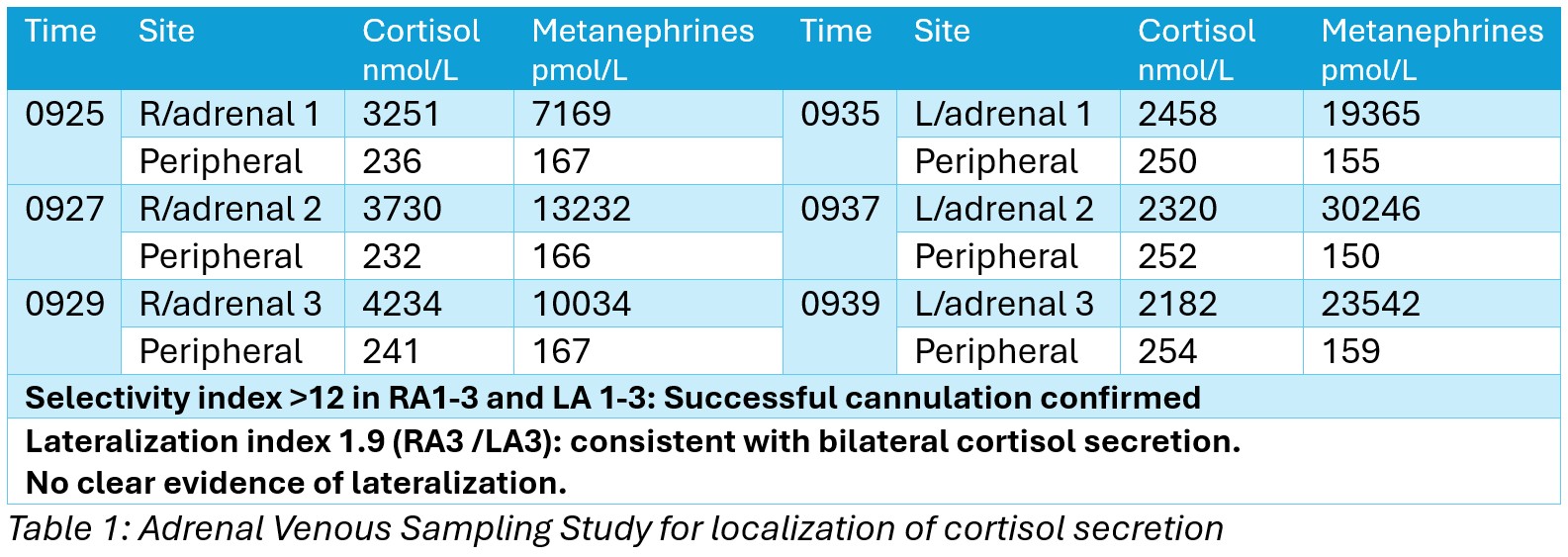
A 55-year-old male with diabetes and poorly controlled hypertension, was found to have bilateral adrenal masses (right: 34x30mm, left:11mm, both with attenuation <-10 Hounsfield units) incidentally detected five years ago on abdominal imaging done for diverticulitis, with normal hormonal profile. Recent repeat imaging showed a 11mm increase in size of the left adenoma albeit retaining lipid-rich morphology. Clinically there was no weight gain, easy bruising, low trauma fractures, headaches or visual disturbances. Repeat biochemistry revealed normal Aldosterone-renin-ratio and plasma metanephrines, however had non-suppressed Overnight Dexamethasone Suppression Test (ODST) of 62 mmol/L raising the possibility of mild autonomous cortisol secretion. Subsequent biochemistry showed evidence of ACTH-independent cortisol hypersecretion (LDDST 58 nmol/L, late night salivary cortisol 9.5 and 10.1nmol/L, 24-hour Urinary-free-cortisol 176 nmol/day, ACTH 6pg/mL). He had worsening blood pressure control and was osteopenic on bone densitometry. Adrenal venous sampling was conducted to localize origin of cortisol secretion, using metanephrines for selectivity index. This showed bilateral cortisol hypersecretion (lateralization index <2).
Given the patient’s relatively young age and established complications likely exacerbated by hypercortisolism, intervention was considered. However, management decisions were constrained by the risks of bilateral adrenalectomy, limited access to cortisol-lowering medications via Pharmaceutical Benefits Scheme (PBS) and the relative toxicity of available therapies. Thus decision was made for aggressive management of complications with close monitoring, with a plan to consider medical or surgical intervention if worsening hypercortisolism.
This case highlights the diagnostic complexity and therapeutic ambiguity posed by bilateral adrenal adenoma with hypercortisolism and importance of individualized treatment decisions.