Poster Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
Severe Prolonged Hypercalcaemia Due to Vitamin D Toxicity: A Case Report (#177)
Introduction
Vitamin D toxicity (VDT) is an uncommon but important cause of hypercalcaemia, increasingly reported due to unregulated supplement use. Management is challenging because of the long half-life and storage of vitamin D in adipose tissue, resulting in prolonged toxicity.
Case Presentation
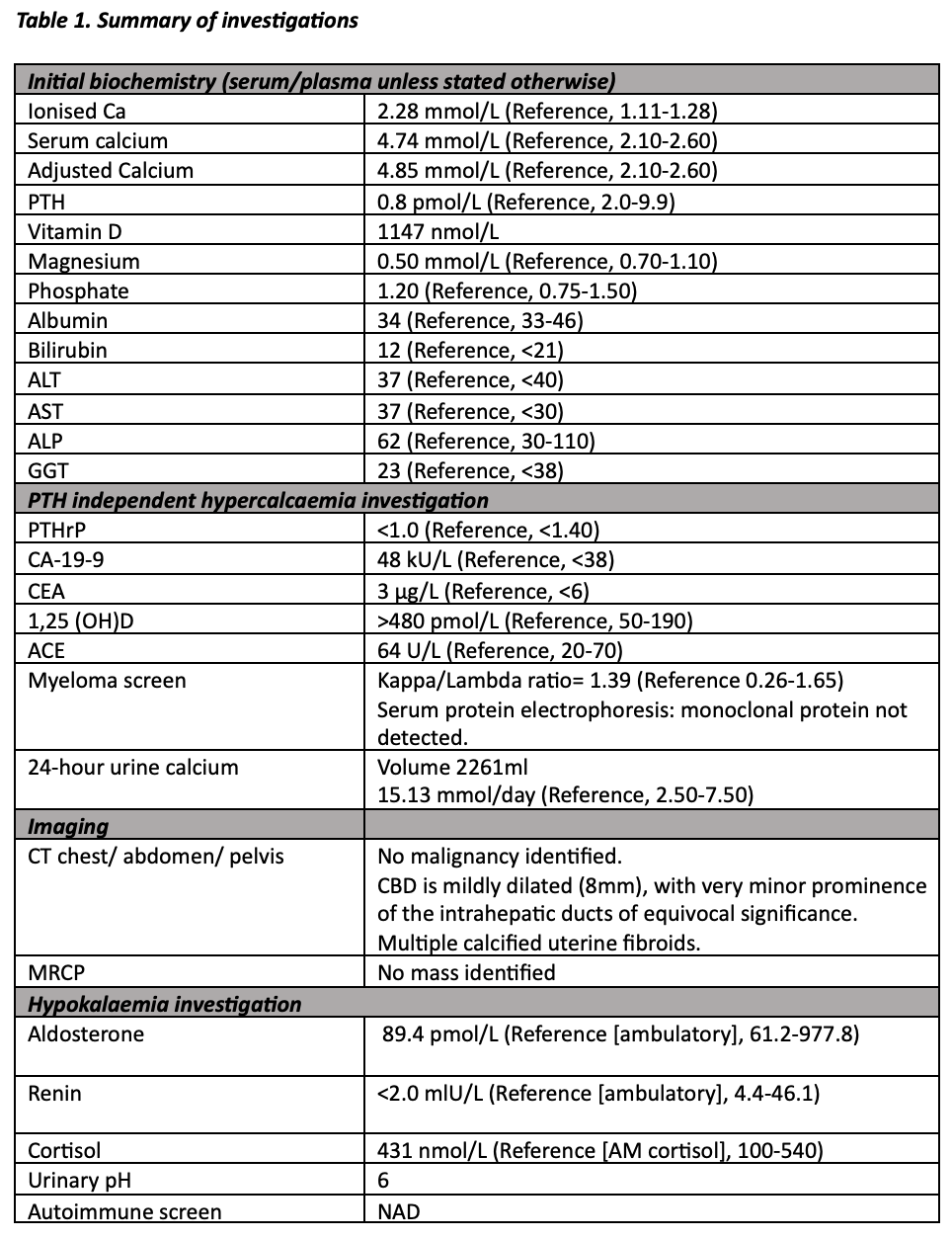
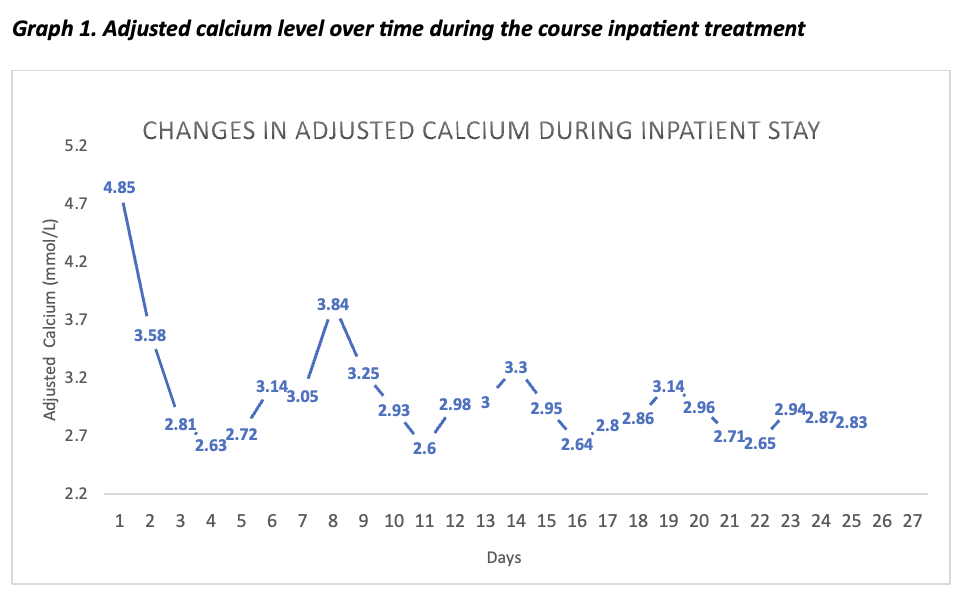
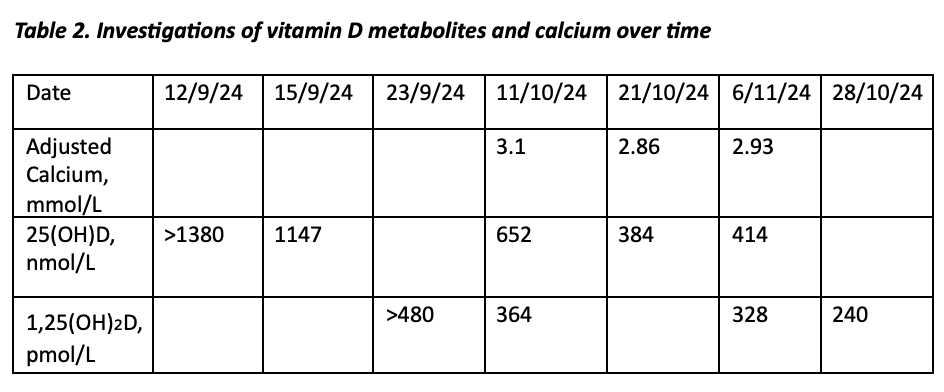
A 68-year-old female presented with two-week history of nausea, fatigue, polyuria, constipation, and confusion. She had been taking herbal vitamin D drops of unknown dose for many years. Investigations revealed severe hypercalcaemia (adjusted calcium 4.74 mmol/L), suppressed PTH (0.8 pmol/L), hypokalaemia (2.9 mmol/L). Serum vitamin D levels were markedly elevated (25(OH)D >1100 nmol/L and 1,25(OH)₂D >480 pmol/L). Extensive work-up excluded malignancy and granulomatous disease (Table 1). The patient received intravenous hydration, potassium replacement, calcitonin, pamidronate, denosumab, and glucocorticoids. Despite these measures, hypercalcaemia persisted for four months, and vitamin D levels normalised only after nine months (Graph 1, Table 2). Hypokalaemia resolved in parallel with declining serum calcium.
Discussion
VTD is defined as 25(OH)D levels greater than 375 nmol/L,1 in this case, levels were over three times higher. VDT primarily increases intestinal calcium absorption, leading to hypercalcaemia.2 The lipophilic nature of Vitamin D causes slow release from hepatic and adipose stores, prolonging hypercalcaemia despite standard therapies.3 Hypokalaemia, likely due to increased distal tubular calcium delivery and potassium wasting was a notable feature.4 Glucocorticoids play a critical role by reducing 1,25(OH)₂D synthesis and intestinal calcium absorption, yet clearance ultimately depends on time.2,5
Conclusion
This case highlights the severe and prolonged nature of hypercalcaemia in VDT, which is often refractory to conventional treatments. Clinicians should counsel patients on the risks of non-prescribed vitamin D use and ensure regular biochemical monitoring. Extended glucocorticoid therapy may be required, and patients should be counselled for a prolonged course. Interdisciplinary collaboration between endocrinology and primary care is essential for long-term management of VDT.