Poster Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
Low K leads the way … but time is short (#179)
Background
Ectopic ACTH syndrome(EAS) is an infrequent but often severe form of ACTH-dependent Cushing’s syndrome. It frequently poses significant diagnostic and management challenges due to atypical presentation and intensity of hypercortisolism.
Case Presentation
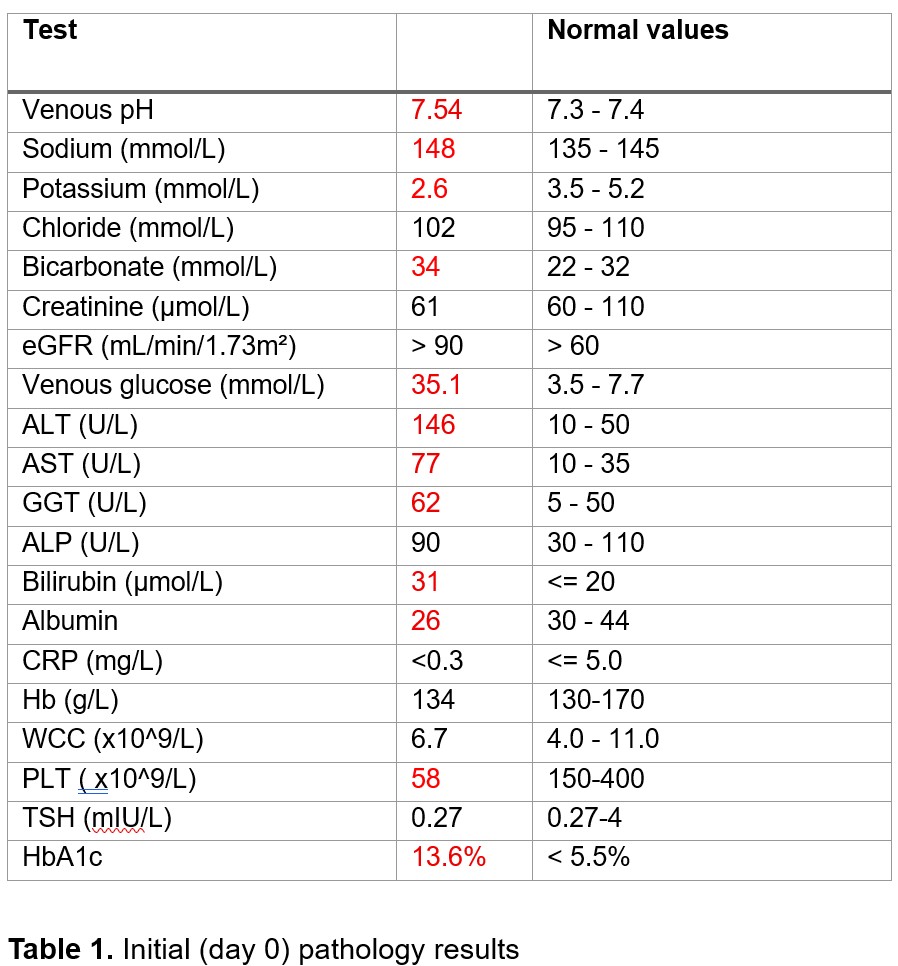
A 74-year-old, previously-well Chinese male presented with fatigue. He was found to have hyperglycaemia, hypokalaemic metabolic alkalosis, thrombocytopenia, and deranged liver function tests(Table 1). He had no Cushingoid features but reported substantial consumption of licorice-containing beverage, raising suspicion for pseudoaldosteronism.
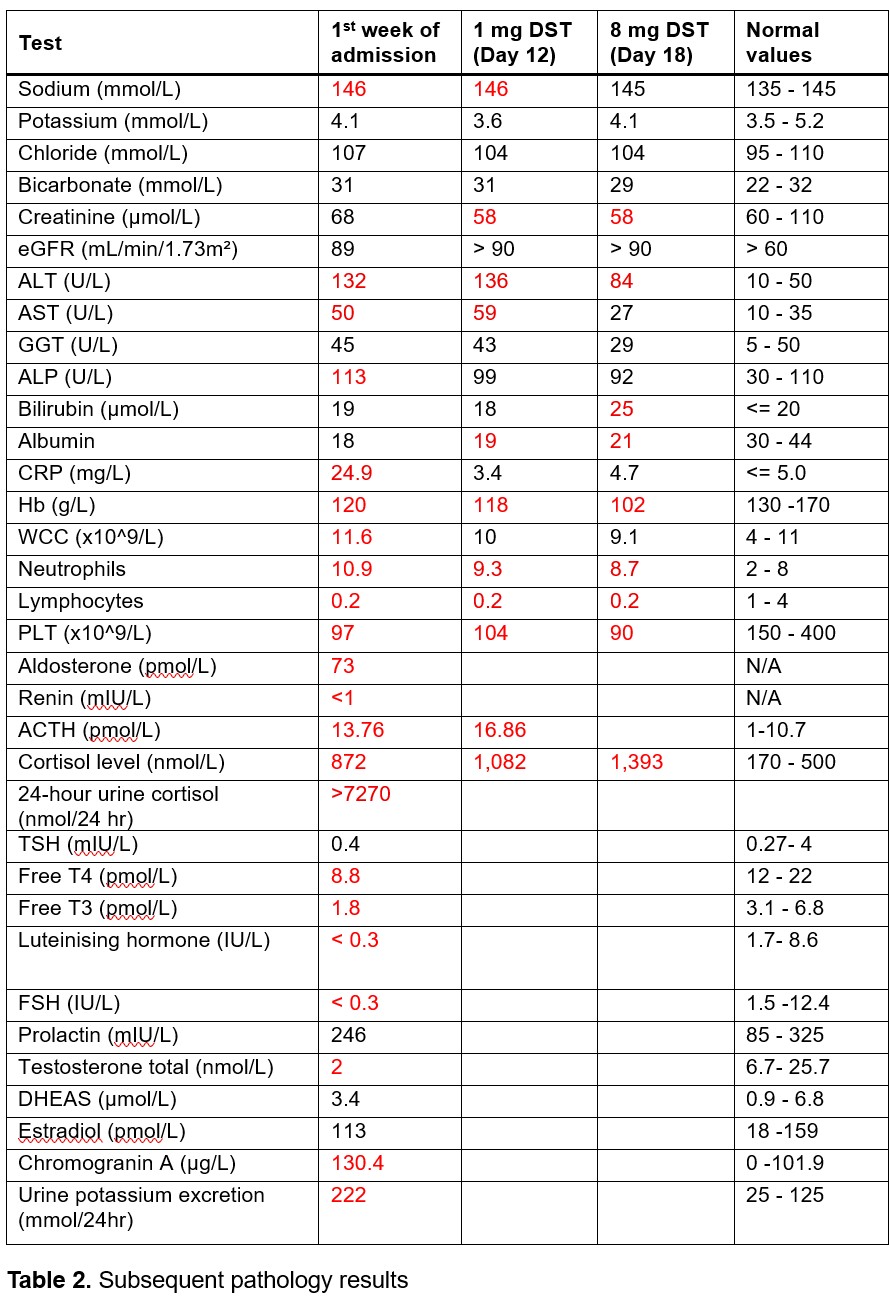
However, further inpatient investigations identified bilateral adrenal hyperplasia and significant ACTH-dependent cortisol excess, which did not suppress with dexamethasone 1mg or 8mg(Table 2). A presumptive diagnosis of EAS was made based on biochemical profile and absence of a pituitary lesion. CT chest revealed rapidly growing pulmonary nodules, raising suspicion for lung malignancy as possible ectopic source of ACTH.
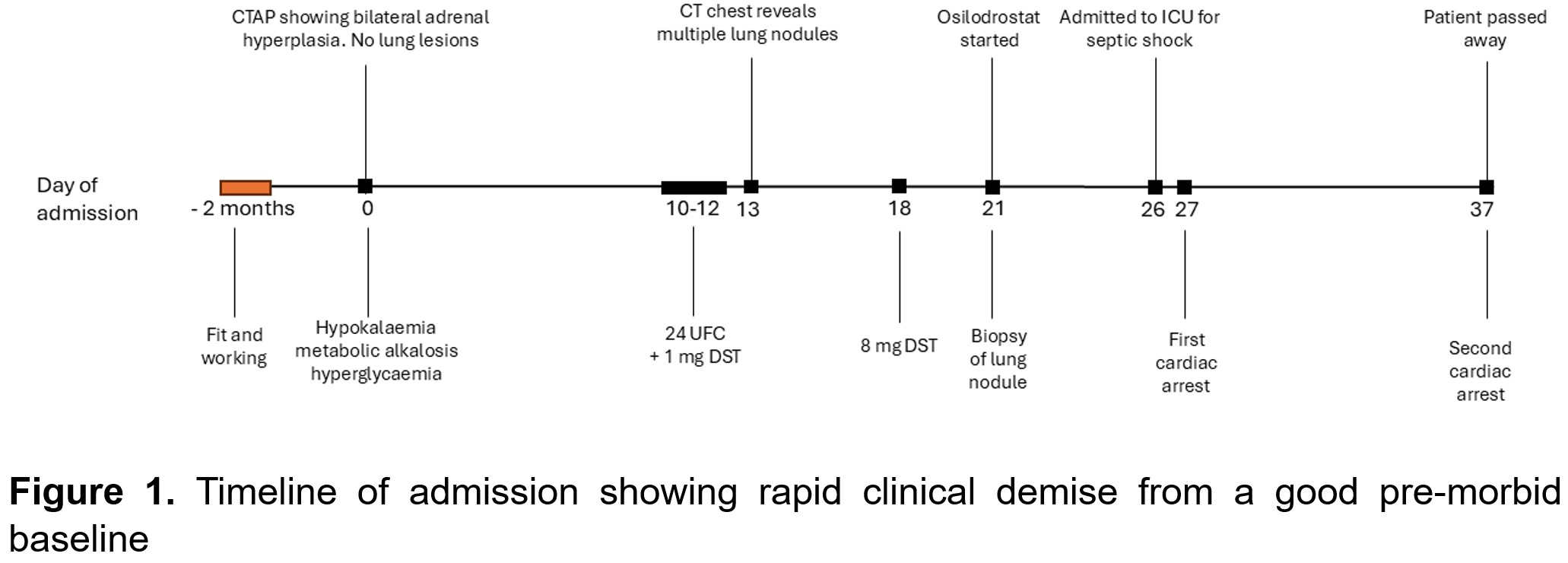
The patient developed progressive myopathy, bruising, and skin thinning. Osilodrostat was commenced as cortisol-lowering therapy. Lung biopsy revealed pulmonary aspergillosis with no malignancy. Pulmonary aspergillosis was compounded by MSSA bacteraemia, leading to septic shock and rapid clinical demise(Figure 1). He died before PET imaging or IPSS could be performed to identify source of presumed EAS.
Discussion
EAS often causes intense hypercortisolism due to unregulated ACTH production by a neuroendocrine tumour.1,2 The intensity of hypercortisolism leads to rapidly accelerated disease course with significant morbidity.1,3 However, EAS diagnosis is often delayed due to atypical presentation with hypokalaemic alkalosis, hypertension and hyperglycaemia, rather than classic Cushingoid appearance.1,4
Osilodrostat is a recently developed steroidogenesis inhibitor which has shown to be effective in rapidly reducing cortisol levels in EAS, though it requires close monitoring of electrolytes, QT-interval and for development of adrenal insufficiency.1,5
Conclusion
EAS should be considered in patients with hypokalaemic metabolic alkalosis, even in the absence of overt Cushingoid signs. Early recognition and aggressive cortisol-lowering therapy are essential to improve outcomes.
- 1. Young J, Haissaguerre M, Viera-Pinto O, Chabre O, Baudin E, Tabarin A. MANAGEMENT OF ENDOCRINE DISEASE: Cushing's syndrome due to ectopic ACTH secretion: an expert operational opinion. Eur J Endocrinol. 2020;182(4):R29-R58. doi:10.1530/EJE-19-0877
- 2. Gadelha M, Gatto F, Wildemberg LE, Fleseriu M. Cushing's syndrome. Lancet. 2023;402(10418):2237-2252. doi:10.1016/S0140-6736(23)01961-X
- 3. Valassi E, Tabarin A, Brue T, et al. High mortality within 90 days of diagnosis in patients with Cushing's syndrome: results from the ERCUSYN registry. Eur J Endocrinol. 2019;181(5):461-472. doi:10.1530/EJE-19-0464
- 4. Howlett TA, Drury PL, Perry L, Doniach I, Rees LH, Besser GM. Diagnosis and management of ACTH-dependent Cushing's syndrome: comparison of the features in ectopic and pituitary ACTH production. Clin Endocrinol (Oxf). 1986;24(6):699-713. doi:10.1111/j.1365-2265.1986.tb01667.x
- 5. Dormoy A, Haissaguerre M, Vitellius G, et al. Efficacy and Safety of Osilodrostat in Paraneoplastic Cushing Syndrome: A Real-World Multicenter Study in France. J Clin Endocrinol Metab. 2023;108(6):1475-1487. doi:10.1210/clinem/dgac691