Poster Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
Do all good things come in pairs? An atypical case of bilateral adrenal masses with cosecretion (#181)
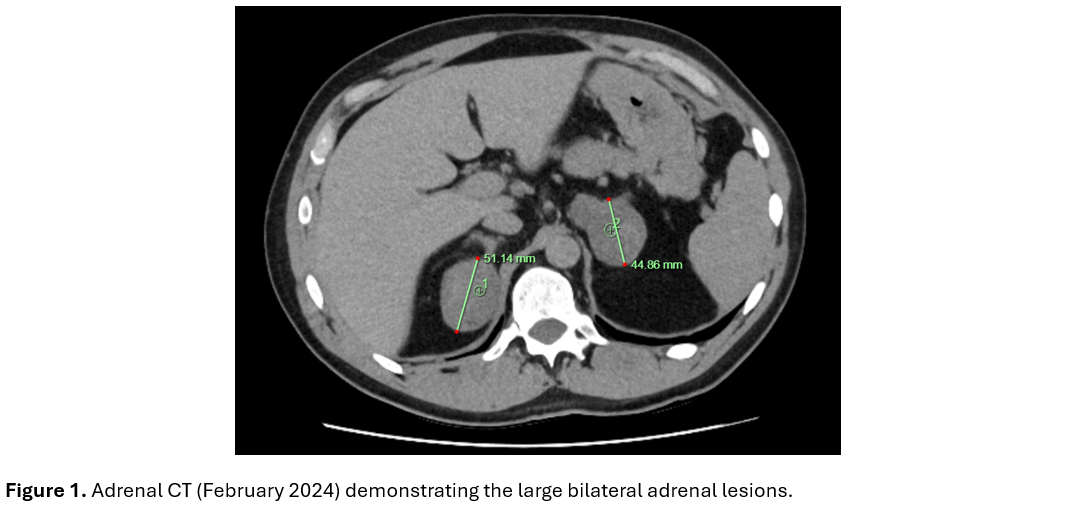
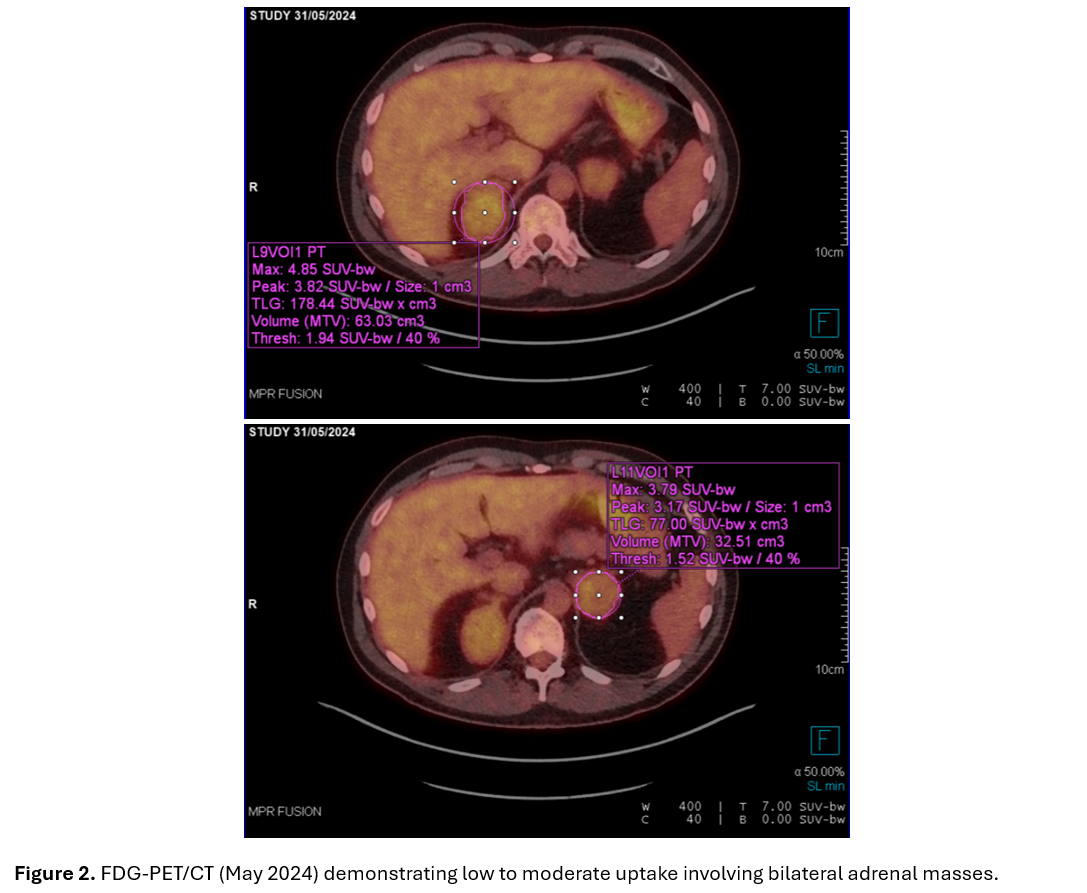
Case summary: A 50-year-old male with a background of familial adenomatous polyposis (FAP), colectomy and loop ileostomy 2002 with high stoma output, presented with large bilateral adrenal lesions (right 57mm, left 59mm) with benign characteristics on CT in 2024(figure 1). Lesions were absent in 2006 and present on CT 2022 (10mm smaller). Malignancy could not be excluded on FDG-PET/CT(figure 2)
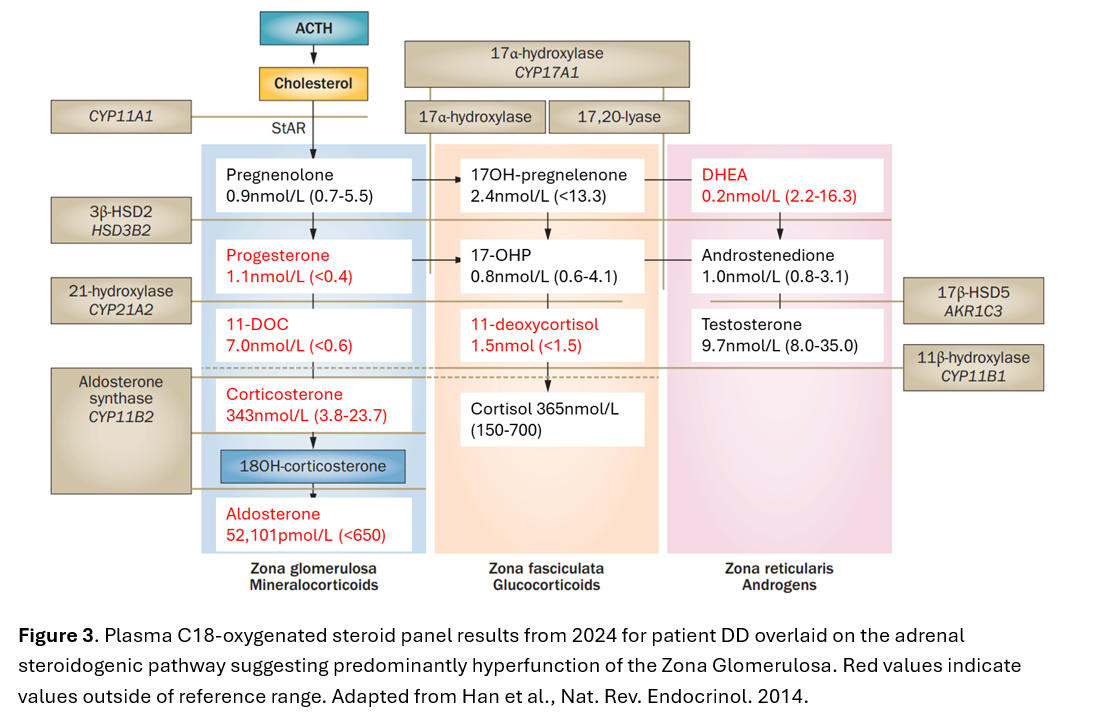
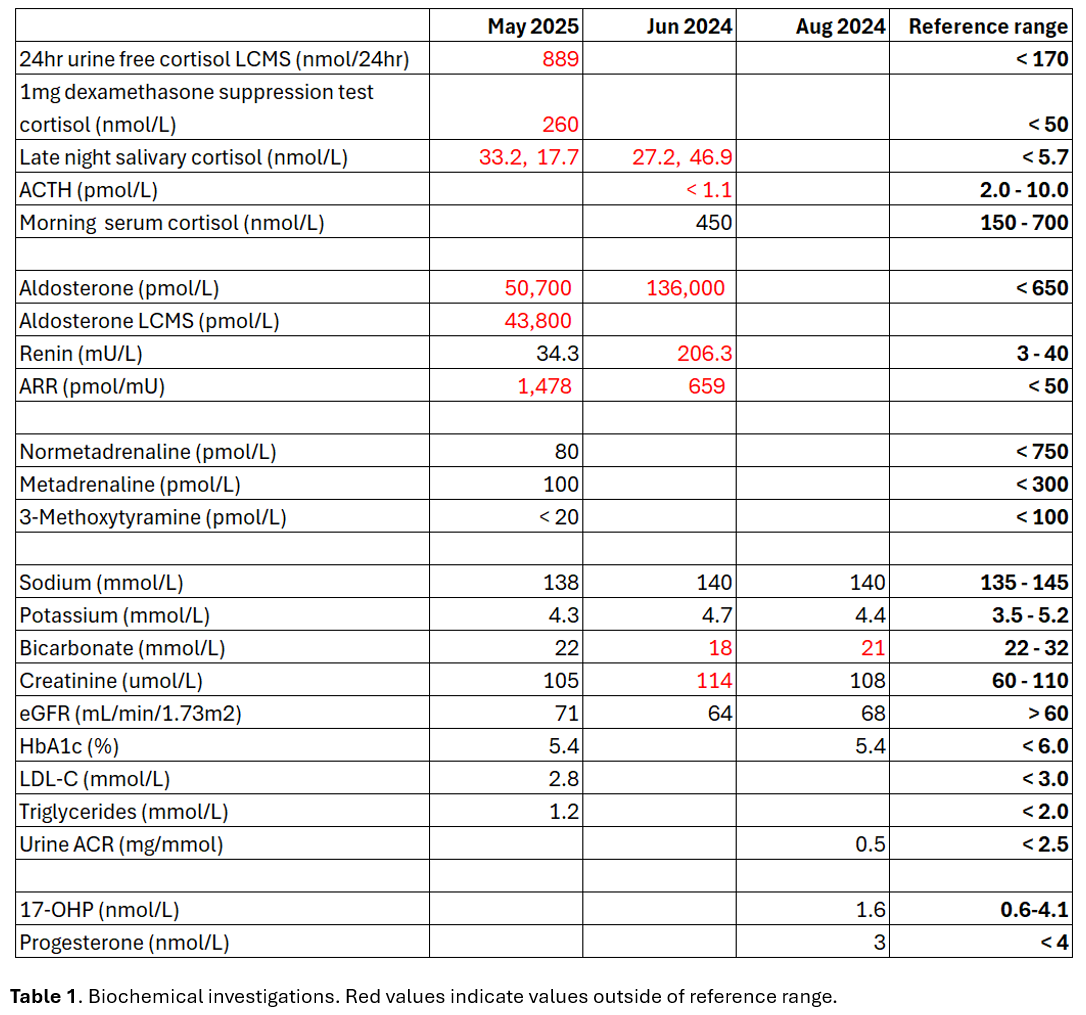
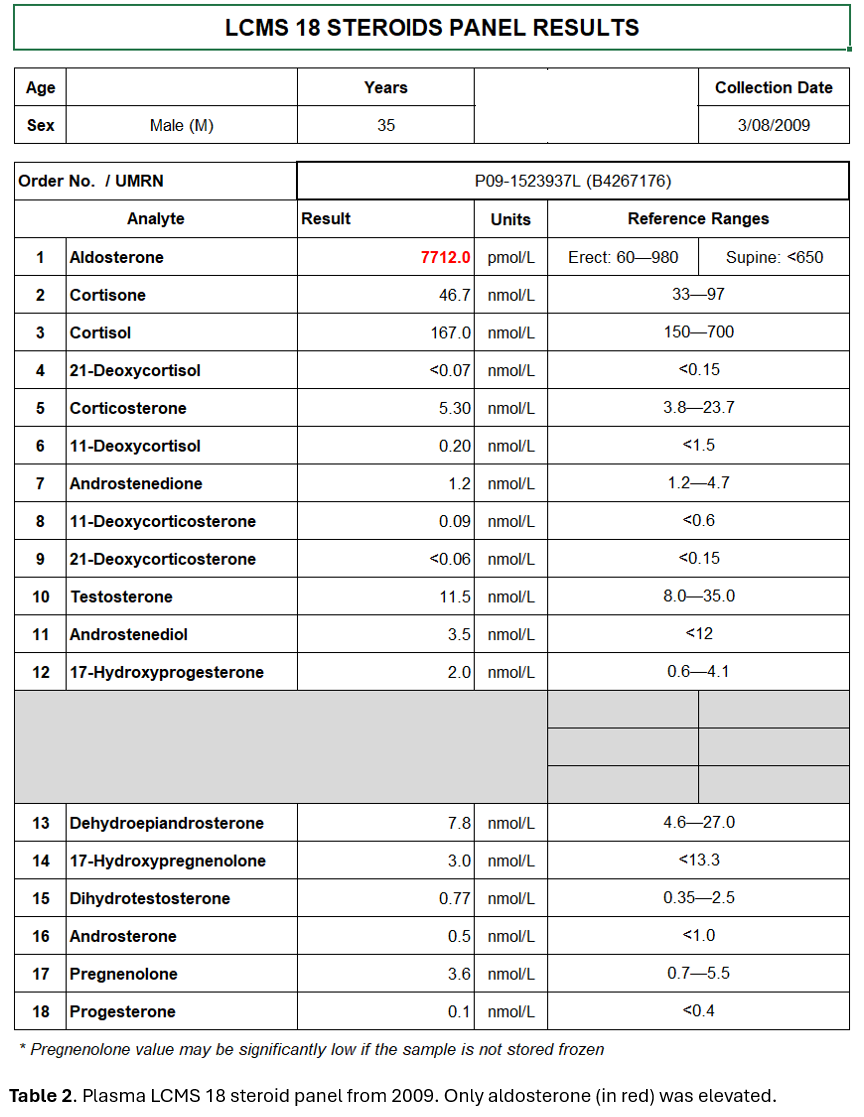
Cosecretion of aldosterone and cortisol was confirmed(table 1). Plasma aldosterone was markedly elevated (50,700, 136,000pmol/L) by immunoassay and confirmed by LCMS(table 1), with unsuppressed renin, elevated ARR and unremarkable sodium and potassium(table 1). An LCMS 18-analyte-steroid-panel measured on a stored serum sample from 2009 demonstrated an isolated elevated aldosterone 7,710pmol/L (an order of magnitude less to 2024)(table 2). The same assay in 2024 demonstrated elevated aldosterone precursors 11-deoxycorticosterone and corticosterone(figure 3). ACTH was undetectable, presumedly suppressed by adrenal metabolites. He had no clinical manifestations of primary aldosteronism or Cushing’s syndrome (besides obesity). Plasma metanephrines were unremarkable
His markedly elevated aldosterone with unsuppressed renin were considered a homeostatic response to decades of unattended high stoma output i.e. longstanding compensatory secondary aldosteronism(1). This process, with his genetic predisposition(2), presumedly lead to the development of large bilateral adenomas and increased secretion of aldosterone precursors. Aldosterone resistance via downregulation of (or defective) intestinal mineralocorticoid receptor (MR) and epithelial sodium channels (ENaC) may be contributory(3,4). MACS was present which is associated with bilateral lesions (5). He was referred to the stoma nurse and is undergoing surveillance for malignant transformation and clinical features of MACS.
Discussion: The physiology of mucosal adaptation and sodium resorption post bowel surgery, mediated by hyperaldosteronism and upregulation of ENaC, will be outlined(1,6,7). Aldosterone resistance in the context of excessive gastrointestinal fluid loss will be explored(3,4). Finally, the associations between FAP and adrenal masses, malignancy and hormone excess will be reviewed(2,8,9,10).
- Koyama K, Sasaki I, Naito H, Funayama Y, Fukushima K, Unno M, et al. Induction of epithelial Na+ channel in rat ileum after proctocolectomy. Am J Physiol. 1999;276(4):G975-84.
- Groen EJ, Roos A, Muntinghe FL, Enting RH, de Vries J, Kleibeuker JH, et al. Extra-intestinal manifestations of familial adenomatous polyposis. Ann Surg Oncol. 2008;15(9):2439-50.
- Vantyghem MC, Hober C, Evrard A, Ghulam A, Lescut D, Racadot A, et al. Transient pseudo-hypoaldosteronism following resection of the ileum: normal level of lymphocytic aldosterone receptors outside the acute phase. J Endocrinol Invest. 1999;22(2):122-7.
- Niyazov D, Shawa H. A Case Of Postileostomy Hypovolemia Presenting As Pseudohypoaldosteronism With Complete Resolution After Ostomy Reversal. AACE Clinical Case Reports. 2017;3(1):e5-e7.
- Vassiliadi DA, Delivanis DA, Papalou O, Tsagarakis S. Approach to the Patient With Bilateral Adrenal Masses. The Journal of Clinical Endocrinology & Metabolism. 2024;109(8):2136-48.
- Rowe KM, Schiller LR. Ileostomy diarrhea: Pathophysiology and management. Proc (Bayl Univ Med Cent). 2020;33(2):218-26.
- Nakamura T, Kurihara I, Kobayashi S, Yokota K, Murai-Takeda A, Mitsuishi Y, et al. Intestinal Mineralocorticoid Receptor Contributes to Epithelial Sodium Channel-Mediated Intestinal Sodium Absorption and Blood Pressure Regulation. J Am Heart Assoc. 2018;7(13).
- Shiroky JS, Lerner-Ellis JP, Govindarajan A, Urbach DR, Devon KM. Characteristics of Adrenal Masses in Familial Adenomatous Polyposis. Dis Colon Rectum. 2018;61(6):679-85.
- Lin L, Beshay V, Macrae F. Adrenal tumours in patients with pathogenic APC mutations: a retrospective study. Hereditary Cancer in Clinical Practice. 2024;22(1):17.
- Johnson Smith TGP, Clark SK, Katz DE, Reznek RH, Phillips RKS. Adrenal masses are associated with familial adenomatous polyposis. Dis Colon Rectum. 2000;43(12):1739-42.