Poster Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
Too big to ignore: a hidden cause of hypoglycaemia (#185)
We present a previously well 49-year-old female referred for evaluation for recent-onset seizure-like episodes occurring over one month. Symptoms included eye-rolling, jerking movements, confusion, and agitation lasting up to 45 minutes. MRI Brain and EEG were normal. She was diagnosed with focal impaired awareness seizures and commenced levetiracetam, but symptoms persisted despite dose escalation. During her second admission, hypoglycaemia (capillary glucose 1.3 mmol/L) was detected, with resolution following intravenous dextrose. She reported progressive abdominal bloating and 4 kg weight gain over 9 months. There was no history of diabetes mellitus, insulin/sulphonylurea use, or relevant family history.
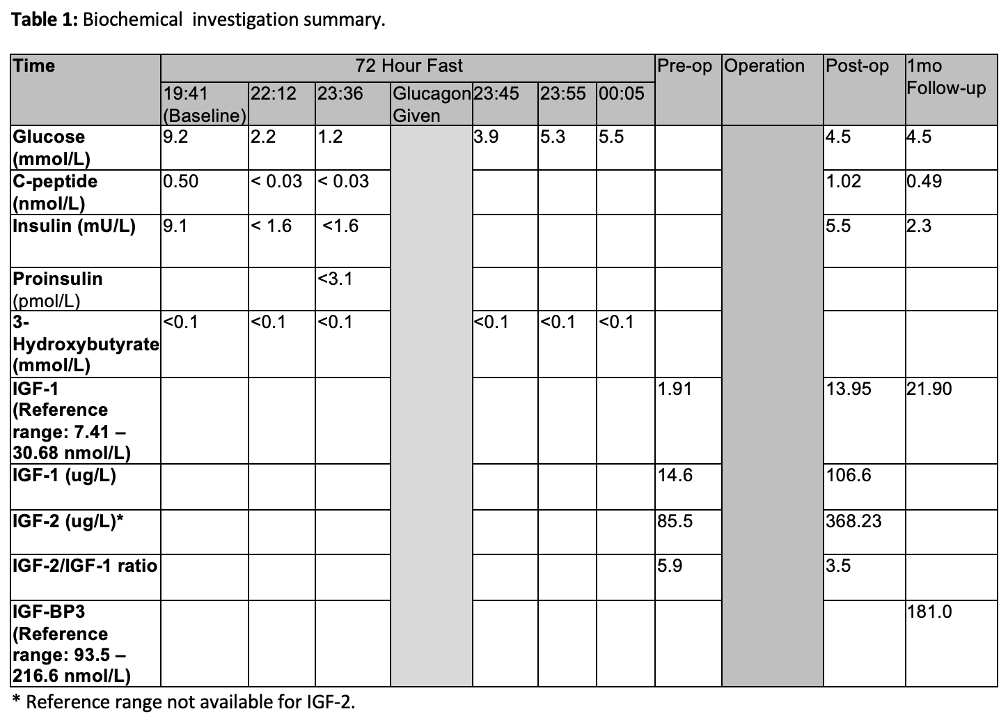
A mixed-meal test and supervised 72-hour fast, which confirmed hypoglycaemia within 4 hours of fasting (Table 1). Biochemistry suggested a non-insulin-mediated cause (suppressed insulin, proinsulin, C-peptide). Persistent hypoglycaemia necessitated intravenous dextrose and glucocorticoids. CT imaging revealed a 156 x 114 x 125 mm left renal mass with central necrosis and normal pancreas, raising suspicion for non-islet cell tumour hypoglycaemia secondary to insulin-like growth factor 2 (IGF-2). She was referred for surgical management.
The patient underwent left renal artery embolization followed by radical nephrectomy (Figure 1). Histopathology confirmed a 130 mm encapsulated solitary fibrous tumour (SFT) confined to the kidney, with adverse-risk features including large tumour size, high mitotic activity, and necrosis. RNA sequencing identified a NAB2-STAT6 fusion, consistent with SFT of intermediate/high-risk (93% 5-year disease-specific survival). Hypoglycaemia resolved immediately post-operatively. At 3-month follow-up, she remains asymptomatic with no evidence of recurrence.

NITCH is rare (1 case/million annually). Diagnosis is based on Whipple’s triad, characteristic biochemistry, tumour identification and resection. SFT-related hypoglycaemia (Doege-Potter syndrome) occurs via high levels of immature IGF-2 secretion (1), which activates insulin receptors, suppresses hepatic glucose production and increases peripheral glucose utilisation. An IGF-2:IGF-1 ratio >10 (normal <3) is suggestive of NICTH (2). Surgical resection remains the only curative treatment.
- Dynkevich Y, et al. Tumors, IGF-2, and Hypoglycemia: Insights From the Clinic, Laboratory, andHistorical Archive. Endocr Rev. 2013;34(6):798–826.
- Ata, F., Choudry, H., Khan, A. A., Anum, Khamees, I., Al-Sadi, A., Mohamed, A., Malkawi, L., & Aljaloudi,E. (2024). A systematic review of literature on Insulin-like growth factor-2-mediated hypoglycaemia innon-islet cell tumours. Endocrinology, diabetes & metabolism, 7(2), e00471.