Poster Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
A decade of discordant thyroglobulin elevation – a case of malignant struma ovarii with thyrotoxic related heart failure (#186)
Malignant struma ovarii is a rare ovarian germ cell tumour containing >50% thyroid tissue, with malignant transformation reported in 5–15% of cases (1). Follicular carcinoma is the most common thyroid-type carcinoma arising in struma ovarii. As in primary differentiated thyroid carcinoma, serum thyroglobulin (Tg), in the absence of anti-Tg antibodies, serves as a reliable tumour marker (2). However, diagnostic and therapeutic challenges arise when Tg remains elevated without localisable structural disease.
We present a 51-year-old female with metastatic malignant struma ovarii, initially diagnosed in 1999 following right oophorectomy for an ovarian teratoma. In 2000, she underwent surgical decompression of a T8 vertebral lesion, revealing metastatic follicular thyroid carcinoma. This prompted total thyroidectomy and radioactive iodine therapy. Histopathology showed entirely benign thyroid tissue, suggesting the struma ovarii as the sole site of malignancy.
Over the following decade, she developed skeletal metastases, including thoracic spine, pubis, jugular foramen and cervical vertebrae, identified on FDG-PET and treated with external beam radiotherapy, most recently in 2015. Tg levels remained chronically elevated (Table 1) with undetectable anti-Tg antibodies, prompting long-term TSH-suppressive thyroxine therapy while she remained asymptomatic.
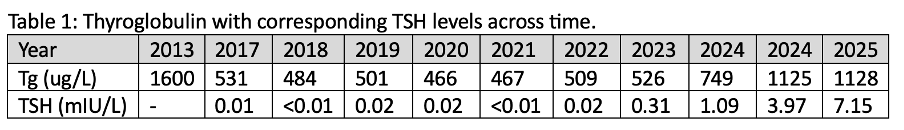
In 2022, she developed atrial flutter and cardiomyopathy with severely-reduced ejection fraction, which resolved post down-titration of thyroxine and normalisation of TSH (heart rate 63 bpm, LVEF 55%). Re-staging scans revealed stable iodine-avid right-sided pulmonary nodules (4mm, 6mm) and osseous metastases (base of skull, C5 transverse process, T8). Given the stability of residual disease, suppressive thyroxine therapy was de-escalated to achieve euthyroidism, correlated with a rise in Tg level (Table 1). Thyroglobulin was sent for mass spectroscopy to confirm rising thyroglobulin concentration despite anatomical and functional scan stability. Bone density was normal.
This case highlights the challenge of rising thyroglobulin despite stable imaging and no symptoms, emphasising the need for personalised decisions about prolonged TSH suppression.
- Lee W, Yi NJ, Kim H, et al. Metastatic follicular struma ovarii complicating pregnancy: a case report and review of the literature. Korean J Hepatobiliary Pancreat Surg. 2012;16(3):123-127. doi:10.14701/kjhbps.2012.16.3.123
- Gild ML, Heath L, Paik JY, Clifton-Bligh RJ, Robinson BG. Malignant struma ovarii with a robust response to radioactive iodine. Endocrinol Diabetes Metab Case Rep. Published online February 14, 2020. doi:10.1530/EDM-19-0130