Poster Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
A Rare Case of Pituitary Macroadenoma - Tuberculous Granulomatous Hypophysitis (#188)
A previously well, 57-year-old male, presented with acute worsening of longstanding headaches, with new onset nausea and vomiting in the setting of Influenza A. Past medical history was significant for investigations into chronic headaches five months prior with magnetic resonance imaging (MRI) demonstrating an enlarged pituitary gland measuring 11mm (Figure 1A). Serum cortisol measured at 10:00 am was 32nmol/L, prompting glucocorticoid replacement. Urgent repeat MRI revealed interval growth in the pituitary lesion to 14mm with contact of the optic chiasm and new central non-enhancement (Figure 1B). On examination, he remained normotensive and afebrile. There were no signs of pituitary hormone excess or visual compromise. Chest examination was normal. Pituitary panel results are summarised in Table 1.
Our patient underwent endoscopic endonasal resection of the pituitary lesion with an uncomplicated recovery (including no AVP-deficiency). Day 8: TSH 0.14 IU/L, FT4 11.4 and FT3 4.5 pmol/L. Testosterone levels are being monitored. Histopathology revealed granulomatous hypophysitis (GRH). A secondary screen for GRH was positive for QuantiFeron-TB (tuberculosis) gold assay (Table 2). Pan computed tomography (CT) studies did not demonstrate other sites of granulomatous disease. Whilst mycobacterium tuberculosis polymerase chain reaction (PCR) is still pending, he has been empirically commenced on anti-microbial therapy, including dexamethasone.
The frequency of pituitary incidentalomas detected on MRI varies from 0.3 to 3% with >80% being adenomatous (1). Of non-adenomatous lesions, the majority represent Rathke’s cleft cysts with hypophysitis accounting for <1% of incidentalomas (1). GRH is therefore extremely rare (2). As its clinical presentation and imaging can mimic adenomas, histological confirmation is crucial (2). GRH can be idiopathic or due to secondary causes including tuberculosis, sarcoidosis, syphilis and vasculitis (2).
In a recent case-series, 60% of patients with tuberculous hypophysitis had evidence of disease elsewhere (3). Our patient is being empirically managed for solitary pituitary involvement.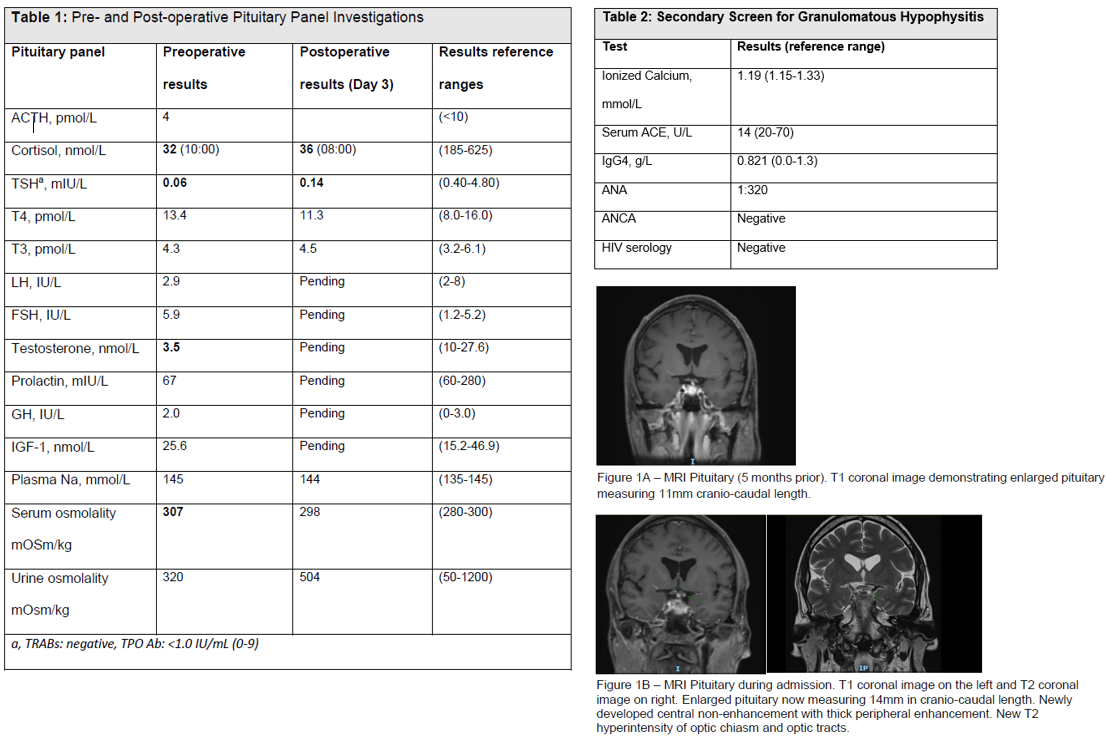
- Fleseriu, M., Gurnell, M., McCormack, A. et al. Pituitary incidentaloma: a Pituitary Society international consensus guideline statement. Nat Rev Endocrinol (2025). https://doi.org/10.1038/s41574-025-01134-8
- Shi J, Zhang JM, Wu Q, Chen G, Zhang H, Bo WL. Granulomatous hypophysitis: two case reports and literature review. J Zhejiang Univ Sci B. 2009 Jul;10(7):552-8. doi: 10.1631/jzus.B0820355.
- Rao A, Lila AR, Karlekar M, Sarathi V, Ban A, Sharma A, Barnabas R, Memon SS, Patil V, Khot W, Sankhe S, Malhotra G, Shah N, Bandgar T. Clinical and radiological insights into secondary hypophysitis: A single-center experience with a focus on tuberculosis. Endocrine. 2025 Jul 8. doi: 10.1007/s12020-025-04352-2.