Poster Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
Co-Design, implementation and evaluation of a nested diabetes model-of-care for adults living with cystic fibrosis (#144)
Aim
Cystic fibrosis (CF) life expectancy is increasing and this is leading to new health challenges, especially diabetes. Nearly 25% of adults with CF develop diabetes, but only a minority receive endocrinology care (1). This study aimed to co-design, implement, and evaluate a nested diabetes model of care (MOC) within a single tertiary adult CF centre in Queensland (2).
Methods
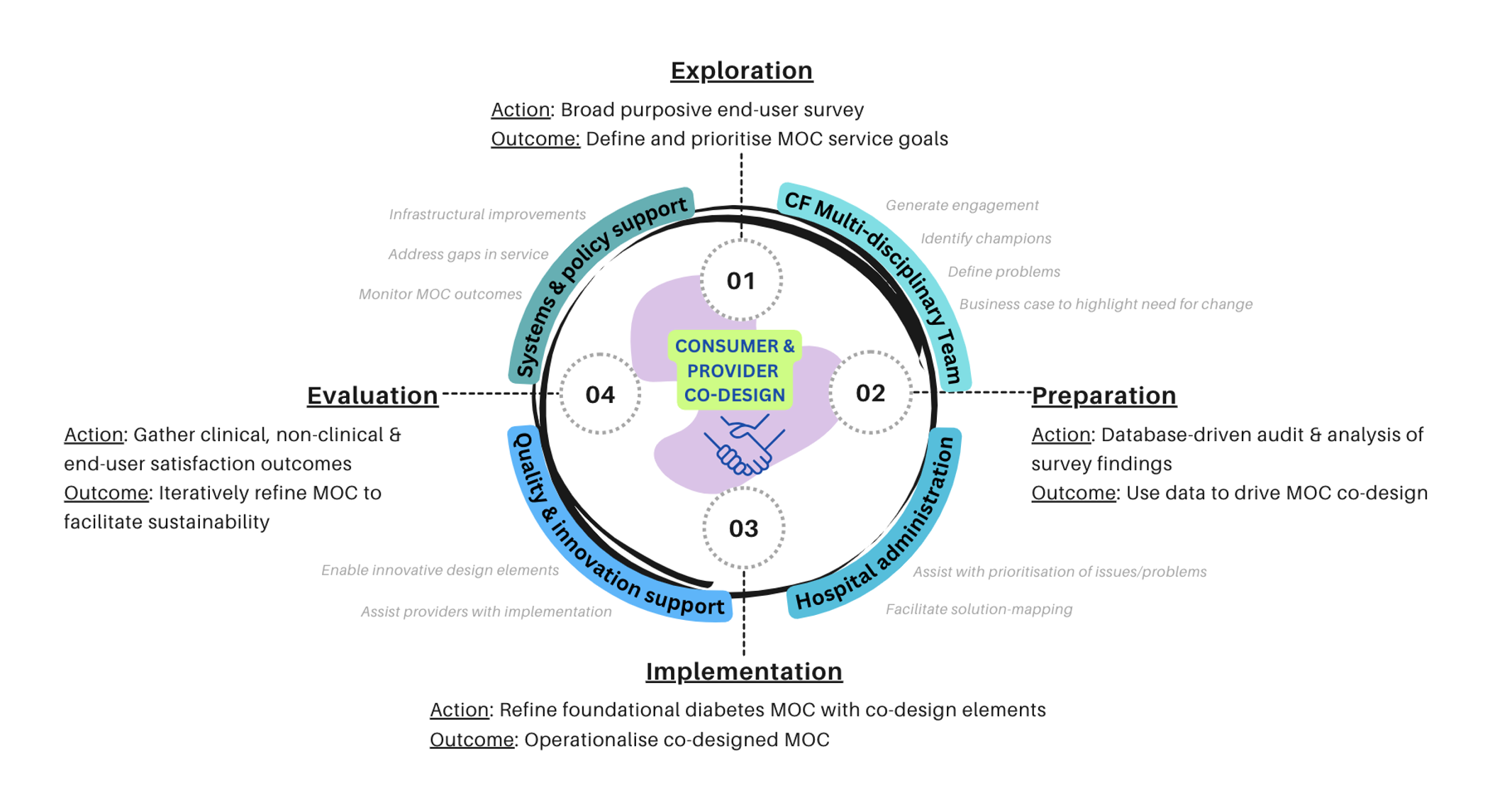
We utilised the Consolidated Framework for Implementation Research to design surveys and workshops for consumer and healthcare provider end-users. We then implemented the co-designed diabetes MOC and used database-driven analytics to evaluate change in primary clinical outcome of HbA1c pre and 12-months post, comparing those who were engaged versus disengaged. A mixed-methods approach was used to evaluate secondary clinical and non-clinical outcomes.
Results
The co-designed diabetes MOC was nested within the pre-existing adult CF services. It promoted multidisciplinary collaboration specifically co-consultations with an endocrinologist, dual credentialed diabetes educator and dietitian. Case conferencing with psychology, social work and other disciplines was also supported. Co-designed referral pathways, flexible diabetes care delivery integrating diabetes technology that supported intensive insulin titration, and co-scheduling of appointments enabled streamlined patient journeys. Our diabetes MOC had high engagement, with 76.7% of our entire CF cohort with confirmed diabetes reviewed within the first year of operationalisation. Engagement with the MOC was associated with a statistically significant decline in HbA1c (-0.54% vs +0.33%, P-value 0.004) and a 0.22% [95% CI 0.19 -0.32] per month increment in percent predicted forced expiratory volume (ppFEV1). End-user satisfaction with the MOC was high.
Conclusion
Our co-designed MOC demonstrated high engagement, improved glycaemic management and lung function in adults with CF living with diabetes. Our approach to CF diabetes care may assist with reducing treatment burden in the order of initiating a new diabetes medication while concurrently enhancing end-user experiences of healthcare.
- Annual Cystic Fibrosis Data Registry (ACFDR) 2023 report. Accessed 18/7/2025 https://www.cysticfibrosis.org.au/wp-content/uploads/2024/07/ACFDR_2023_Annual-Report.pdf
- Kumar, Shanal and Smith, Daniel and Moore, Vanessa and Matson, Angela, Co-Design, Implementation and Evaluation of a Nested Diabetes Model-of-Care for Adults Living with Cystic Fibrosis. Available at SSRN: https://ssrn.com/abstract=5048730 or http://dx.doi.org/10.2139/ssrn.5048730