Oral Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
Socioeconomic differences in the cost-effectiveness of a telephone-based intervention for obesity prevention in early childhood (128164)
The aim of this study was to investigate in different socio-economic groups, the cost-effectiveness of an early childhood obesity prevention intervention providing telephone and short message service (SMS) support to mothers of children aged 2-4 years (1). Socio-economic position (SEP) was defined as high or low, based on annual household income. A modelled SEP-specific economic evaluation of the intervention was conducted, using a microsimulation model (2) to predict SEP-specific body-mass index (BMI) trajectories, prevalence of overweight and obesity, quality-adjusted life years (QALYs) and health care costs until 17 years of age. SEP-specific intervention costs and effects at age 5 years were derived from the trial data and applied to a cohort of 4- to 5-year-old Australian children. Incremental cost-effectiveness ratios (ICERs) and acceptability curves were derived for each SEP group, using 2023 Australian dollars.
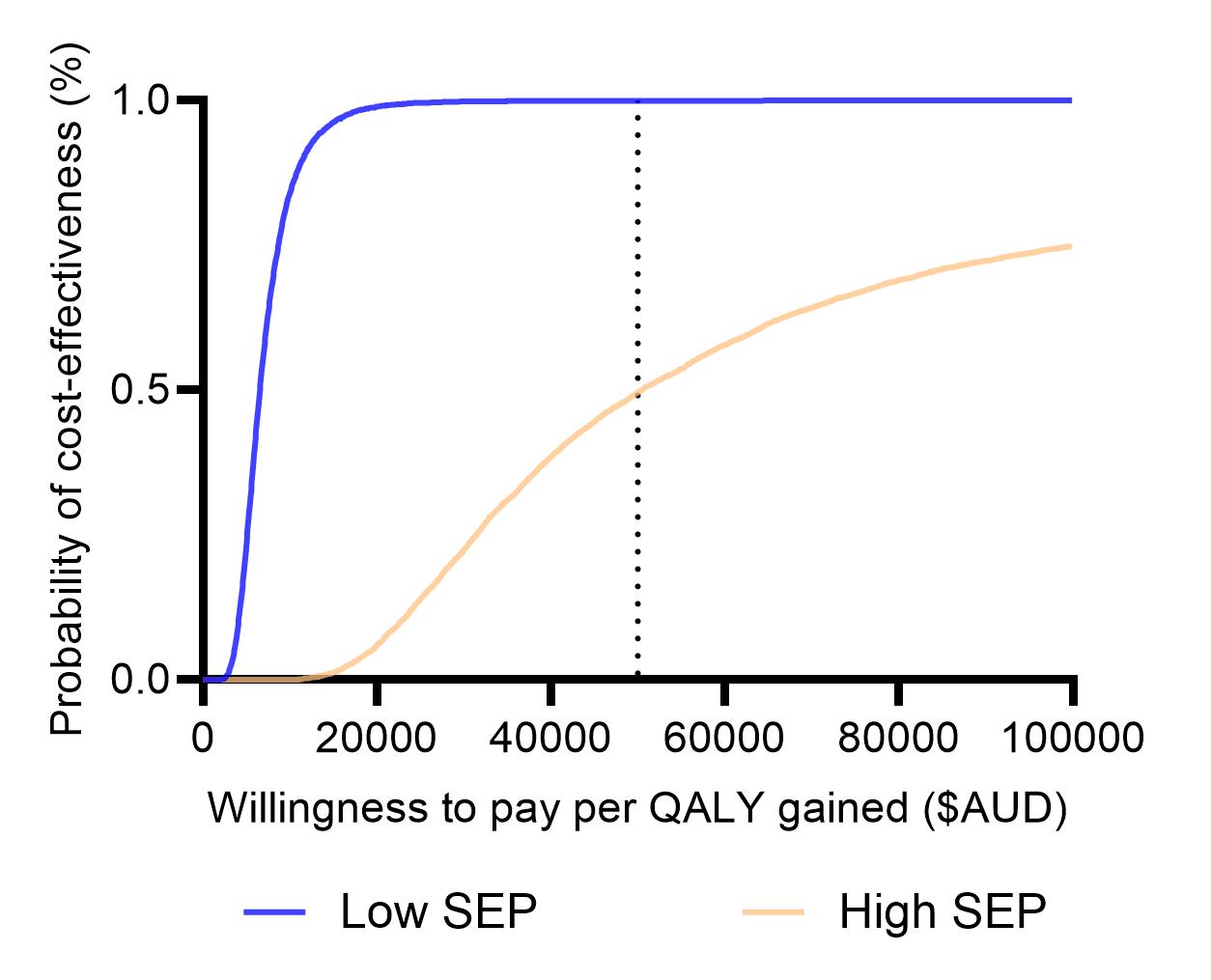
The model predicted, at age 17 years, that the intervention could reduce overweight and obesity in the low SEP group from 58% to 40% and in the high SEP group from 52% to 49%. From an Australian health payer perspective, the ICERs for the low-SEP group were $131 per BMI unit avoided and $6,549 per QALY gained, compared to the high-SEP group at $1,161 per BMI unit avoided and $41,462 per QALY gained. Results were robust to sensitivity analyses varying the intervention effect size, intervention costs, healthcare costs, discount rate and disutility from overweight. The probability that the intervention was cost-effective at a willingness-to-pay threshold of $50,000 per QALY gained was extremely high in the low-SEP group (99.7%) and marginally cost-effective in the high-SEP group (49.6%) (Figure). The greater cost-effectiveness in the lower SEP group suggests that prioritizing families from socioeconomically disadvantaged backgrounds for this service will represent good value for money and may reduce healthy weight inequalities in childhood.
- 1. Li Ming Wen, Huilan Xu, Zoe Chen, Alison Hayes, Philayrath Phongsavan, Sarah Taki, Erin Kerr, Danielle Jawad, Lisa Simone, Chris Rissel, and Louise Baur. Effectiveness of a telephone-based randomised clinical trial targeting obesity risk of preschool-aged children: An extension study during the COVID-19 pandemic. Accepted International Journal of Obesity, June 2025.
- 2. Killedar A, Lung T, Taylor RW, Taylor BJ, Hayes A. Is the cost-effectiveness of an early-childhood sleep intervention to prevent obesity affected by socioeconomic position? Obesity (Silver Spring). 2023 Jan;31(1):192-202