Oral Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
From Crisis to Coordination: Impact of a Structured Obesity Treatment Program on Health Service Utilisation (128281)
 Evaluating a 12-month, three-phase, rapid weight-loss and weight stabilisation, multidisciplinary service (TOMS) for efficiencies of care for patients living with complex obesity.
Evaluating a 12-month, three-phase, rapid weight-loss and weight stabilisation, multidisciplinary service (TOMS) for efficiencies of care for patients living with complex obesity.
Participants commencing in the TOMS program from January 2021 to May 2023 had tertiary healthcare occasions of service (OOS) recorded for the 12-month period prior to, and 12-month period post program completion. OOS included emergency presentations, admissions, bed days and outpatient appointments. For these outcome measures, incidence ratios (IR) were calculated pre and post TOMS. Counts of emergency and outpatient care for specific conditions and allied health specialties were compared using McNemar’s test.
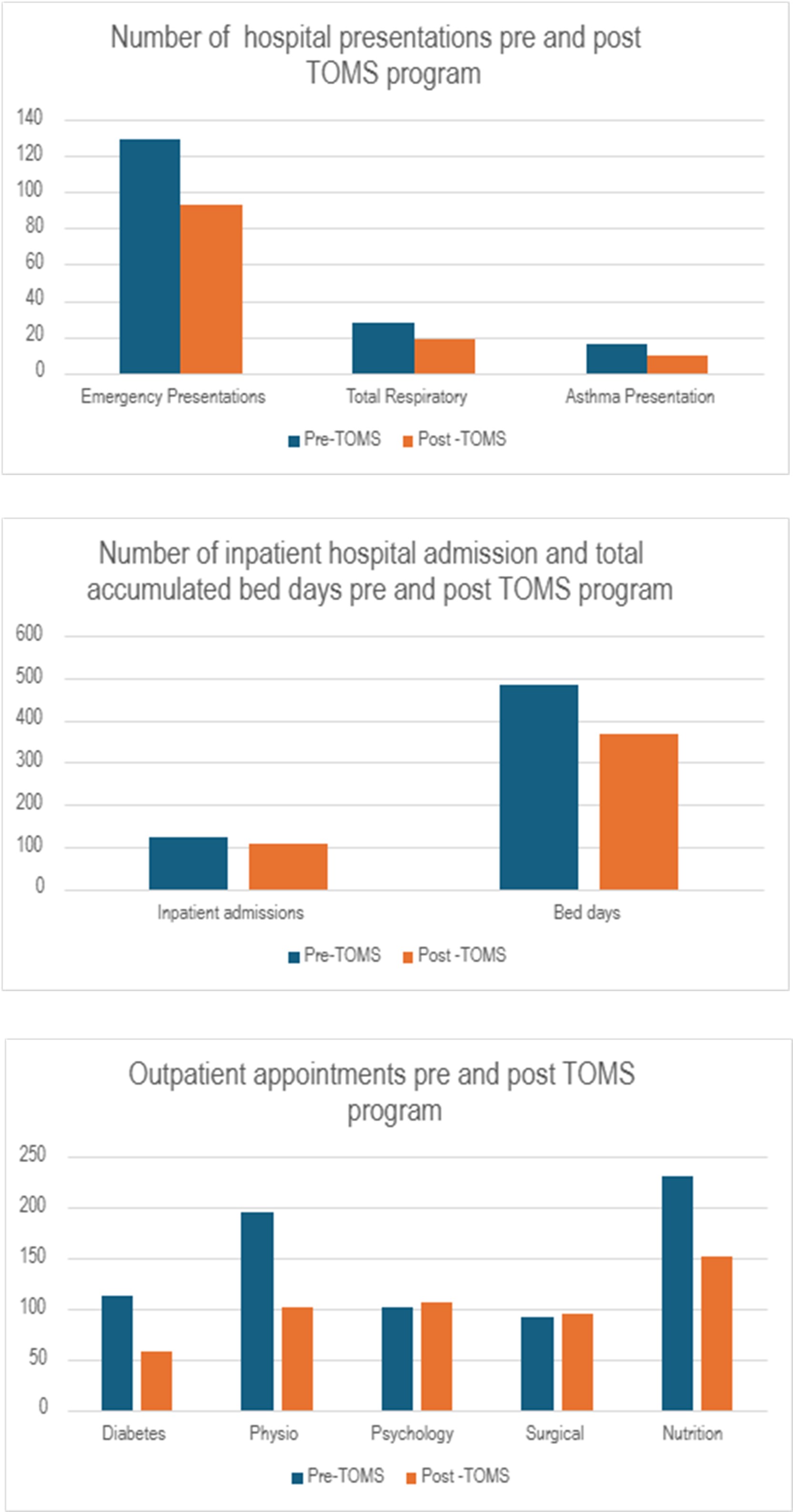
A total of 119 patients commenced TOMS during the study period; median BMI 46.4kg/m2 (40.5-54.8kg/m2). Emergency presentations reduced by 28% (IR=0.72) from 129 to 93 post-TOMS. Of these, total respiratory presentations (including asthma) reduced by 20.7% (95%CI 12.2, 29.2) and asthma presentations reduced by 29.7% (95%CI 21.8, 37.7). Inpatient admissions decreased from 125 to 109 post-TOMS, a 13% reduction (IR 0.87), total bed days decreased by 25% (IR 0.75) from 484 to 366 after TOMS. Total outpatient appointments of 1759 pre- and 1248 post-TOMS, decreased by 28% (IR 0.72), including a 35.9% (95%CI 33.9-37.9%) decrease in diabetes appointments. Dietetics, pharmacy and physiotherapy appointments reduced by 28.8% (95%CI 26.6, 30.9), 35.0% (95%CI 33.0, 37.0) and 31.7% (95%CI 29.6, 33.8) respectively post-TOMS. Psychology appointments increased by 34.6% (95%CI 32.7, 36.5) and surgical outpatient appointments increased by 35.2% (95%CI 33.4, 37.2) post TOMS.
TOMS participation was associated with reduced overall healthcare utilisation, with greater use of psychology and surgical appointments post-TOMS indicating improved access to care in these areas. Future research could calculate the health economic benefits of TOMS.