Oral Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
ANZ interdisciplinary survey of non-functioning pituitary adenoma management: areas of variability and common practice (128687)
Aim:
To determine ‘real-world’ current practices in NFPA investigation and management across Australia and New Zealand (ANZ), comparing to the recent consensus guidelines from the Pituitary Society on pituitary incidentalomas and helping guide future initiatives.
Methods:
An anonymous online survey comprising four clinical scenarios (23 questions total) was disseminated to ANZ consultant endocrinologists, neurosurgeons and rhinologists via the ANZRS, ANZSB, ESA, NSA and NZSE.
Results:
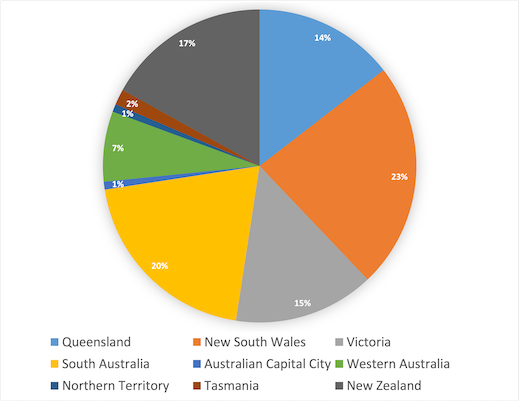
99 endocrinologists and 25 surgeons (11 neurosurgeons, 14 rhinologists) across ANZ responded (Fig.1).
In relation to intrasellar microadenomas:
- Gadolinium was requested for MRI assessment by 66% of all responders#
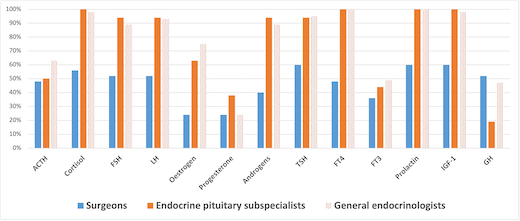
- Hormonal evaluation included cortisol, FSH, LH, androgens (for males), TSH, fT4, prolactin and IGF-1 by > 90% of endocrinologists. ACTH was requested by 61%# (Fig.2)
- Growth hormone was regularly requested (87% surgeons vs 42% endocrinologists)*#
- Repeat MRI evaluation was requested at 2+ years by 6% of total responders#
- Surgeons requested formal visual field testing more frequently (52%# vs 19%)*
For asymptomatic macroadenomas clear of the optic chiasm:
- 16% of all responders organised repeat imaging at 12 months#
For macroadenomas with associated visual deficit:
- Surgeons referred more often for MDT evaluation (72% vs 47%#)*
- Cortisol was most consistently checked day 3 post op
- Full post operative hormonal evaluation was performed at 4-6 weeks (46% surgeons vs 89% endocrinologists)*
- Repeat was most commonly requested 3 months post operatively (64% surgeons vs 39% endocrinologists)*
Statistically significant variability also existed between endocrinologists who attended regular pituitary MDTs and MDT clinics vs general endocrinologists.
# Areas of discordance with consensus recommendations
* Areas with statistically significant differences between specialists
Conclusions:
This large survey dataset (n=124) identifies areas of deviation and concordance in real-world practice from recent guidelines, highlighting areas for improvement as well as unmet needs within current recommendations.