Oral Presentation ESA-SRB-ANZOS 2025 in conjunction with ENSA
Habitual dietary intake does not predict micronutrient deficiencies in individuals with Diabetes-Related Foot Ulcers: Analysis from the VITAFOOT Pilot Trial (128079)
Micronutrients such as Vitamin C and Zinc are important in all phases of wound healing, including in collagen synthesis and epithelialisation(1). Deficiencies are common in individuals with Diabetes-Related Foot Ulcers (DFU)(2). The Australian Short Dietary Screener (AUS-SDS) assesses average daily intake across six food groups and is validated in an elderly Australian population(3). We aimed to determine average dietary intake across food groups and correlation to micronutrient deficiencies in individuals with DFU.
The VITAFOOT Study is a pilot randomised control trial investigating the effect of a combination micronutrient supplementation on ulcer healing in patients with DFU. Participant diet across the domains of fruit, vegetables, legumes/beans, cereal/grains, protein and dairy sources was evaluated at baseline using the AUS-SDS(3). Daily equivalent frequencies (DEFs)were calculated for each food group, with 1 DEF representing one serve per day. Plasma Vitamin C and Zinc levels were recorded at enrolment.
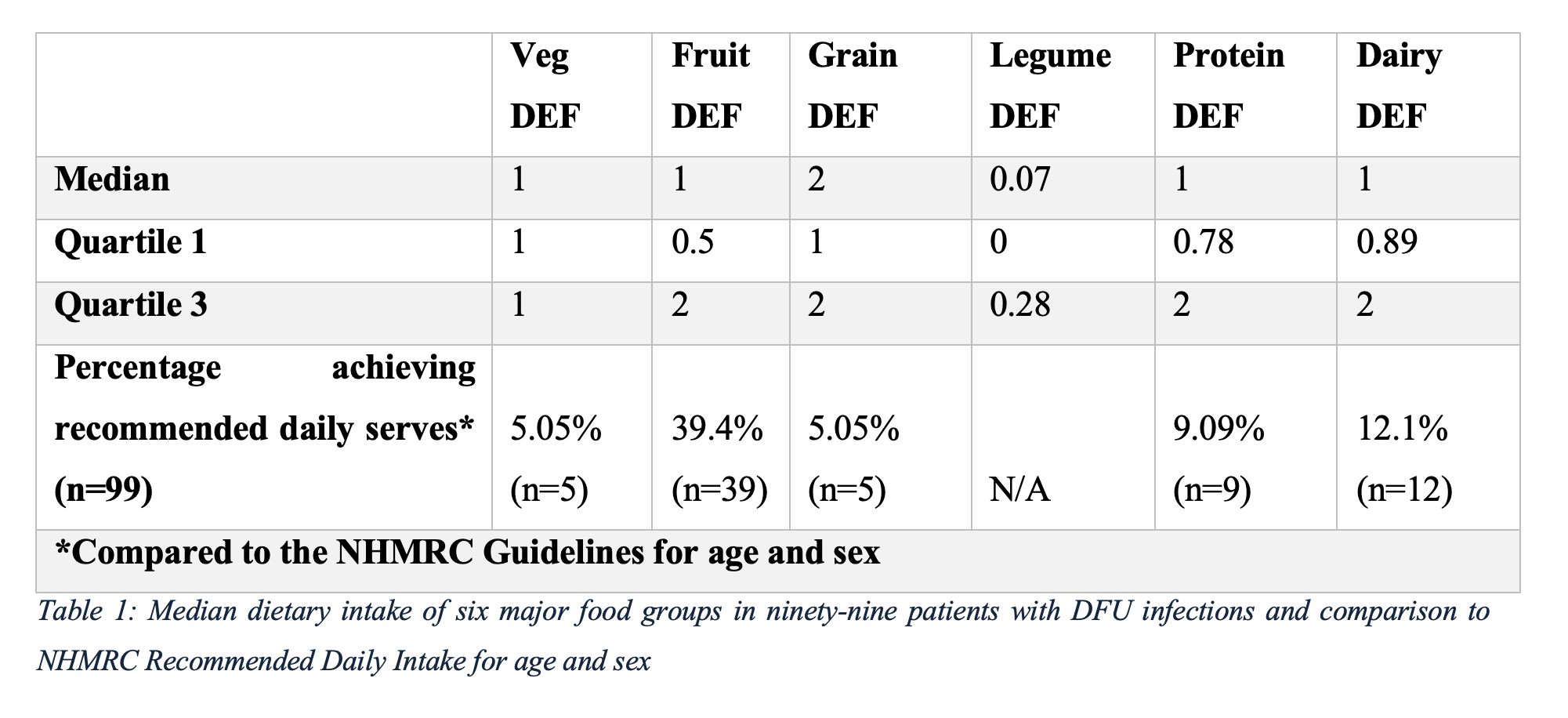
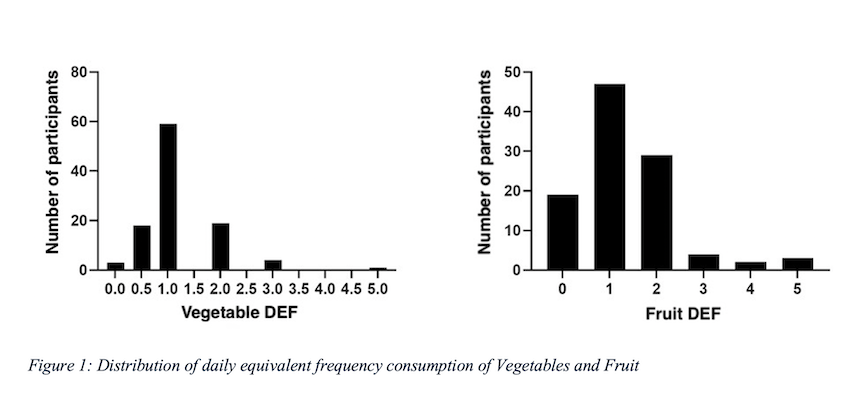
Ninety-nine participants completed the AUS-SDS. Median [interquartile range] intakes were 1 [1-1] DEF vegetables, 1 [0.5-2] DEF fruit, 2 [1-2] DEF dairy, 0.07 [0-0.28] DEF legumes/beans, 1 [0.78-0.2] DEF protein sources and 1 [0.89-2] DEF dairy sources. For any food group, less than 40% of participants met intake recommendations (4). Eighty-nine participants had plasma Vitamin C and 96 plasma Zinc levels recorded at enrolment. No significant correlations were observed between reported intake of any food group and plasma Vitamin C or Zinc levels. There was no difference in vegetable (p=0.27) or fruit (p=0.11) intakes between those who were Vitamin C replete versus deficient (plasma Vitamin C <4µmol/L).
Average daily intake of all food groups amongst participants with a DFU was below the recommended intake for Australian adults, indicating suboptimal diet quality(4). The lack of significant correlation between dietary intake and micronutrient levels suggests factors additional to diet contribute to nutritional deficiency in this high-risk population.
- 1. Ghaly P, Iliopoulos J, Ahmad M. The role of nutrition in wound healing: an overview. Br J Nurs. 2021;30(5):S38-S42. doi:10.12968/bjon.2021.30.5.S38
- 2. Pena G, Kuang B, Cowled P et al. Micronutrient Status in Diabetic Patients with Foot Ulcers. Adv Wound Care, 2019;9(1). doi: 10.1089/wound.2019.0973
- 3. Gadowski AM, McCaffrey TA, Heritier S, et al. Development, Relative Validity and Reproducibility of the Aus-SDS (Australian Short Dietary Screener) in Adults Aged 70 Years and Above. Nutrients. 2020;12(5):1436. Published 2020 May 15. doi:10.3390/nu12051436
- 4. Australian Government National Health and Medical Research Council. Recommended number of serves for adults. Eat For Health. Accessed July 18, 2025. https://www.eatforhealth.gov.au/food-essentials/how much do we need each day/recommended number serves adults